Understanding Gastric Sleeve Surgery:
Your Foundation for The Cure Holiday All-Inclusive Gastric Sleeve Journey:
A Path to Sustainable Health and Wellness Change
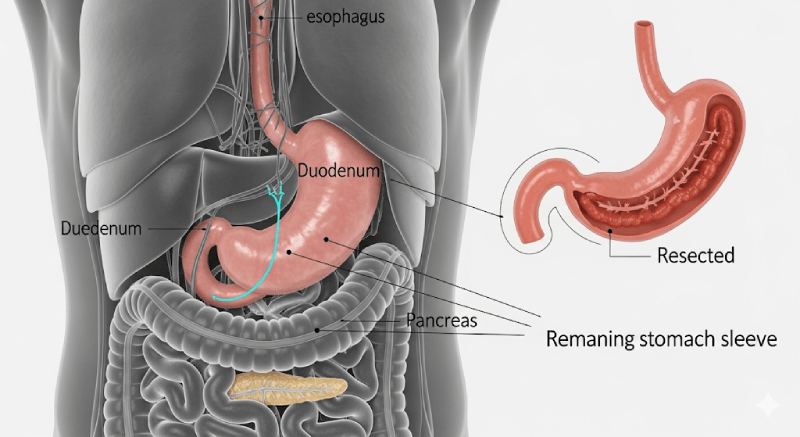
Definition and Mechanism of Sleeve Gastrectomy
Gastric Sleeve surgery (Sleeve Gastrectomy) is a definitive clinical treatment designed for individuals diagnosed with morbid obesity. This minimally invasive procedure is performed laparoscopically under general anesthesia. During the operation, approximately 75% of the stomach is surgically removed, creating a thin, vertical pouch, or “sleeve”. This mechanism primarily restricts the amount of food that can be consumed in one sitting, leading to satiety with smaller portions. Crucially, by removing the section of the stomach responsible for producing ghrelin, the hunger hormone, the procedure also aids in appetite regulation, supporting long-term success. The laparoscopic approach uses small incisions, minimizing tissue damage, scarring, and significantly shortening the post-operative recovery time—a key benefit for international patients.
Expected Transformations in Health and Weight Loss
This surgery is not merely a weight loss tool; it is a comprehensive intervention aimed at resolving severe, obesity-related health issues. Patients can expect substantial weight loss, leading to dramatic improvements in overall health and quality of life. Benefits extend to improved conditions such as Type 2 Diabetes (insulin resistance), severe hypertension, and sleep disorders. Reduced body weight increases mobility, relieves joint pain, and decreases the long-term risk of serious health problems, including heart disease, stroke, and certain cancers. On a psychosocial level, patients often report improved self-confidence and mental well-being. Achieving these lasting results, however, is deeply dependent on the patient’s commitment to a dedicated post-operative diet and exercise regimen.
Eligibility: Clinical and Lifestyle Readiness
Clinical Criteria for Bariatric Intervention
Gastric Sleeve surgery requires strict adherence to medical criteria, as it is a major intervention. Eligibility is primarily determined using the Body Mass Index (BMI).
BMI Calculator
Your BMI:
Primary Candidates: Individuals with a BMI of 40.0 or higher are generally considered candidates without needing additional obesity-related health issues.
Candidates with Comorbidities: Individuals with a BMI between 35.0 and 39.9 are eligible if they have one or more serious obesity-related conditions (comorbidities), such as poorly controlled Type 2 Diabetes, hypertension, or severe sleep apnea. This criterion underscores that the surgery’s goal is to mitigate life-threatening risks associated with excessive weight.
| BMI Range (kg/m²) | Associated Comorbidity Status | Eligibility Assessment |
| BMI ≥40.0 | No additional obesity-related health issues required. | Generally Eligible |
| BMI 35.0−39.9 | One or more severe comorbidities (e.g., Type 2 Diabetes, Severe Hypertension, or Sleep Apnea) required. | Eligible with Comorbidities |
| BMI <35.0 | Generally not considered a primary candidate for surgical intervention. | Requires Special Review |
The Importance of Comprehensive Preparation
Success depends on being psychologically and behaviorally prepared, as the surgery is the start of a permanent lifestyle commitment. The pre-operative phase mandates necessary medical testing to ensure clinical suitability. Crucially, patients must eliminate high-risk habits, specifically smoking and alcohol consumption, before the operation. Quitting smoking is vital as it improves wound healing and reduces the risk of post-operative complications like pulmonary issues and gastric leaks. A disciplined preparation phase, which includes a specific pre-operative diet to shrink the liver, confirms the patient’s readiness for long-term compliance.
The Cure Holiday Advantage:
Value, Quality, and Seamless Travel
Accessible Costs Without Compromising Quality
Cure Holiday offers world-class medical services at a significantly lower cost compared to Western nations. While the average cost of this procedure ranges from $15,000 to $25,000 in the United States and $10,000 to $18,000 in Western European countries like the UK or Germany , our package model typically falls within the estimated range of $3,500 to $5,500. This structural difference allows patients to achieve savings of up to 70% compared to US/European pricing. This efficiency is achieved without compromising the quality of care, providing exceptional value by combining expert surgical skill with economic advantage.
| Region | Estimated Average Procedure Cost (USD) | Estimated Savings with Cure Holiday |
| United States (USA) | $15,000 – $25,000 | 70% or More |
| Western Europe (UK/Germany) | $10,000 – $18,000 | 50% – 70% |
| Cure Holiday Destination (Estimated Range) | $3,500 – $5,500 | N/A (Baseline Cost) |
Clinical Excellence and Advanced Infrastructure
Our partner hospitals feature state-of-the-art medical infrastructure and are staffed by highly skilled surgeons. Many of these specialists have trained at leading global medical centers and utilize the most advanced surgical techniques and technology. The mature medical tourism industry in our destinations means that the entire process is optimized for the international patient, offering comprehensive, integrated services. This focus includes professional language interpreter services, comfortable accommodation, and efficient airport transfers, ensuring a smooth and stress-free journey.
Pre-Surgical Preparation:
Setting the Stage for Success
The Clinical Pre-Assessment Phase
The pre-operative phase is a mandatory step to ensure physiological suitability and procedural safety. This includes performing all necessary medical tests and diagnostic screenings to confirm the patient is fit for surgery and to identify any potential risks. Patients must adhere strictly to a pre-operative diet program designed to reduce the size of the liver, which is often enlarged in obese individuals. A smaller liver improves the surgeon’s visibility and enhances safety during the laparoscopic procedure. Strict adherence to lifestyle restrictions, such as ceasing alcohol and tobacco use, is confirmed during this time.
Hospital Admission and Immediate Preparation
Hospital admission typically takes place on the morning of the surgery, unless an existing health condition requires earlier admittance. The most crucial pre-operative rule is the NPO (Nil Per Os) status: the patient must not consume anything, including water, after midnight the night before the surgery. Upon arrival, patients should bring personal items and any regular medications. The admission process involves multiple checks of identity, medical history, and procedure details by various staff members. Though repetitive, these safety protocols are essential for high corporate safety standards, ensuring accuracy and controlled progress. After final preparations, the patient is dressed in surgical attire, transferred to the operating room, where monitoring equipment is attached, and anesthesia is administered.
Treatment and Stay Logistics:
Your Timeline for Travel and Recovery
Hospital Stay and Acute Recovery
The standard hospital stay post-Gastric Sleeve surgery is 4 nights. This duration is vital for acute post-operative monitoring, allowing for the early detection and management of potential complications like bleeding or leakage. During this time, the patient’s hydration is stabilized, and the initial clear liquid diet phase begins under careful medical supervision. Before discharge, the patient must demonstrate the ability to manage hydration, mobilize, and successfully complete the mandatory nutritional education session provided by the bariatric dietitian.
Total Cure Holiday Stay and Local Recuperation
While the hospital stay is 4 nights, the recommended total time to remain in the destination country is generally 7 to 10 days. The days following discharge are crucial for continued healing, adaptation to the new restrictive diet, and full stabilization. Traveling long distances immediately after major abdominal surgery can increase the risk of deep vein thrombosis (DVT) and severely impact patient comfort. The extended 7 to 10-day local recovery period ensures safe adjustment to the diet program and clinical stability before undertaking a long flight.
Comprehensive Package Inclusions
(The Cure Holiday Model)
Core Surgical and Medical Services
Cure Holiday packages offer financial transparency by covering all essential costs directly related to the surgical procedure:
- Professional Fees: Services of the lead bariatric surgeon and the anesthesiology team.
- Hospital Care: Facility fees for the operating room and the mandatory 4-night hospital stay for acute care and monitoring.
- Medical Essentials: All necessary pre-operative diagnostic tests and initial post-operative medications for pain management and reflux control.
- Nutritional Support: Initial consultations and a detailed post-operative diet plan created by the bariatric team, critical for long-term success.
VIP Logistics and Support Services
We eliminate the logistical stress of medical travel so you can focus entirely on your recovery:
- Private Transfers: Dedicated, personalized transportation services for all essential trips, including airport, hospital, and hotel transfers.
- Communication Support: Professional language interpreter services are provided throughout the hospital stay to ensure clear communication with the medical team.
- Safety Assurance: As part of our commitment, mandatory travel insurance is included in the package price. Including travel insurance is a critical safeguard in medical tourism, mitigating patient concerns about potential medical emergencies far from home.
Post-Operative Roadmap:
Managing Recovery Stages
Adhering strictly to the post-operative nutrition plan is the most critical factor determining the long-term success of the procedure. This plan mandates a gradual transition and permanent behavioral changes.
Key Rules for Nutritional Success
Two fundamental nutritional rules must be followed for life: prioritize high protein intake and maintain the separation of solids and liquids.
- Protein Requirement: To support healing, preserve muscle mass, and target body fat for weight loss, high daily protein targets must be met. This is typically 80-85 grams per day for women and 90-100 grams per day for men.
- Separation of Solids and Liquids: This is a permanent, non-negotiable rule: Patients must wait at least 30 minutes after consuming solid food before drinking any liquid, and vice versa. This separation is clinical—drinking with meals washes food out of the small restrictive sleeve too quickly, nullifying the restrictive effect, increasing the risk of overeating, and causing digestive discomfort. Compliance is vital for sustaining long-term weight loss.
Gradual Nutritional Adaptation Program
The recovery and gastric adaptation process is divided into four distinct, progressive nutritional phases.
Clear Liquid Diet (Post-Op Days 1-2)
The primary goal of this initial phase is to rest the stomach staple line and ensure hydration to prevent dehydration. Intake is strictly limited to water, clear broths, and non-pulpy, sugar-free, transparent liquids. All carbonated beverages, caffeine, and solid foods are strictly prohibited.
Full Liquid Diet (Approximately 2 Weeks)
Immediately following the Clear Liquid Diet, this phase lasts for about two weeks. The goal is to safely transition to more nutritious liquids while meeting protein goals. Acceptable intake includes thin, sugar-free protein shakes, strained creamy soups, and other high-protein liquids.
Puree Diet (Approximately 2 Weeks)
This phase, lasting roughly two weeks, aims to introduce thicker, blenderized consistencies while maintaining high protein intake. All foods must be completely smooth (baby-food consistency) with no chunks or hard fibers to prevent obstruction. Examples include pureed cottage cheese with potato , soft vegetables, and pureed fish.
Low-Fat Soft Solids (Starting Week 5 Onwards)
This is the phase where lifelong eating habits are permanently established. The focus is on incorporating chewable, moist protein sources, such as soft meats, fish, and eggs. Patients will gradually introduce more challenging foods, like raw vegetables and dried legumes, later in this phase. Foods high in fat and simple sugars must be strictly avoided. Calorie-dense items like nuts should typically be introduced only after 2-3 months and under the supervision of a bariatric dietitian.
| Diet Phase | Typical Post-Op Duration | Primary Goal | Key Restrictions |
| Clear Liquid Diet | Days 1 – 2 | Hydration and resting the surgical site. | Absolutely no sugar, carbonated drinks, or solid food. |
| Full Liquid Diet | Approximately 2 Weeks | Meeting protein goals while ensuring gastric tolerance. | Only smooth, strained liquids (protein shakes, thin soup). |
| Puree Diet | Approximately 2 Weeks | Transitioning to thicker textures; introduction of blenderized proteins. | Food must be a completely smooth puree; no chunks or hard fiber. |
| Low-Fat Soft Solids | Starting Week 5 Onwards | Establishing lifelong healthy eating habits; reinforcing solid/liquid separation. | Avoidance of high-fat foods, simple carbohydrates, and initially, tough textures. |
Long-Term Lifestyle Integration and Follow-Up
Managing Weight Loss Expectations and Timeline
Weight loss dynamics post-sleeve surgery vary, but patients typically experience the fastest rate of loss within the first 6 months. The majority of the expected total weight loss occurs within the first year following the procedure. This timeline helps manage expectations, shifting the focus from rapid initial loss to continuous, long-term weight management after the first 6-12 months. Regular integration of physical activity is crucial alongside nutrition to maintain muscle mass, boost metabolism, and enhance overall mobility.
Remote Monitoring and Lifetime Commitment
The success of bariatric surgery requires continuous medical and nutritional follow-up, often transcending geographical boundaries. Patients are expected to maintain periodic remote consultations with the bariatric team and coordinate care with their home country physician. Due to rapid weight loss and restricted intake, patients must adhere to a lifelong protocol of vitamin and mineral supplementation to prevent deficiencies. Addressing the psychological and emotional adjustments that come with rapid body change and new eating patterns is also a vital component of sustaining emotional health and preventing weight regain. Cure Holiday provides structured, ongoing remote support to bridge this critical gap after the patient returns home.