IVF Gender Selection
In vitro fertilization (IVF) has evolved from a treatment for infertility into a platform for a range of advanced reproductive technologies, including gender selection. The only scientifically reliable method for determining a child’s sex prior to conception is Preimplantation Genetic Testing (PGT) performed in conjunction with IVF. This advanced process allows for the identification of an embryo’s sex with nearly 100% accuracy, providing a level of control over reproductive outcomes previously unattainable. The practice is motivated by a diverse set of factors, ranging from uncontroversial medical imperatives to prevent the transmission of sex-linked genetic disorders to more debated elective reasons, such as “family balancing” or personal preference.
The availability and legality of elective gender selection vary dramatically across the globe, creating a fragmented legal landscape. While many Western nations, including the United Kingdom and Australia, strictly prohibit the procedure for non-medical reasons, a number of other countries have adopted more permissive policies, establishing a robust global market for medical tourism. This disparity in legal frameworks and a significant difference in costs—with procedures in medical tourism hubs being a fraction of the price of those in the United States—are the primary drivers of cross-border patient flow. The practice remains at the center of an intense ethical debate, balancing an individual’s right to reproductive freedom against societal concerns related to the commodification of children, the reinforcement of gender bias, and the potential for a “slippery slope” toward genetic enhancement.
The Science and Mechanism of Gender Selection
In Vitro Fertilization (IVF): A Foundational Overview
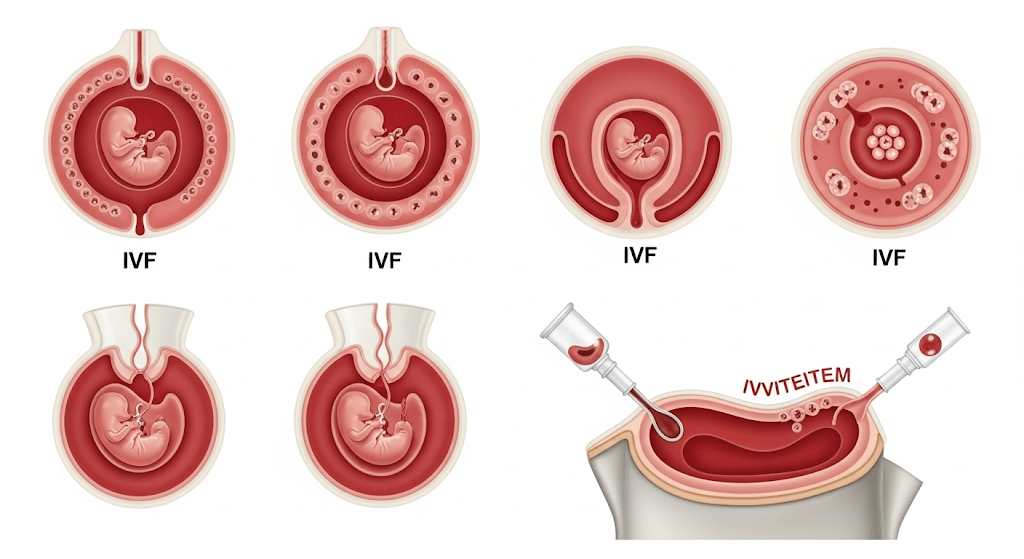
Gender selection is not a standalone procedure but rather a sophisticated add-on to the established process of In Vitro Fertilization (IVF). The process begins with ovarian stimulation, where the prospective mother or egg donor self-administers medication to encourage the ovaries to produce multiple mature eggs. When the eggs are deemed ready, they are retrieved in a minimally invasive outpatient procedure guided by ultrasound.
Following retrieval, the eggs are fertilized with sperm in a laboratory setting. This can be achieved through conventional fertilization, where sperm and egg are combined in a petri dish, or through a technique called Intracytoplasmic Sperm Injection (ICSI), where a single sperm is injected directly into the egg. Once fertilized, the embryos are cultured and closely monitored as they develop over a period of three to six days. This culturing period is critical as it allows the embryos to reach a sufficient stage of development—the blastocyst stage—for the subsequent genetic testing. A key step in this process, and a prerequisite for gender selection, is the embryo biopsy, where a highly skilled embryologist removes a small number of cells from the outer layer of the embryo, known as the trophectoderm. This biopsy procedure is considered safe and does not significantly impact the embryo’s ability to develop.
Preimplantation Genetic Testing (PGT): The Core Mechanism
Preimplantation Genetic Testing (PGT) is the scientific cornerstone of modern gender selection. PGT is a broad term that encompasses two distinct types of testing, Preimplantation Genetic Diagnosis (PGD) and Preimplantation Genetic Screening (PGS), which are often used together in a single cycle.
- Preimplantation Genetic Diagnosis (PGD): This test is utilized when there is a known family history of a specific genetic disease. PGD allows clinicians to identify harmful gene mutations for conditions such as cystic fibrosis, hemophilia, Huntington’s disease, or Tay-Sachs disease before an embryo is implanted. This is considered a critical tool for couples at high risk of passing on a known genetic disorder.
- Preimplantation Genetic Screening (PGS): Also known as PGT for Aneuploidy (PGT-A), this test screens for chromosomal abnormalities, or aneuploidy, which involve having too many or too few chromosomes in the embryo’s DNA. Chromosomal irregularities are a leading cause of miscarriage and can result in conditions such as Down syndrome, Edward syndrome, and Turner syndrome. PGS is particularly beneficial for older women, as the incidence of chromosomal irregularities increases significantly with maternal age, from 30-40% in women under 30 to 70-90% in women over 40.
Crucially, both PGD and PGS can identify the sex of an embryo by analyzing its sex chromosomes—XX for a female embryo and XY for a male embryo. This shared capability is what enables gender selection as an ancillary, and often elective, application of PGT.
Success and Accuracy: Separating Gender Identification from Live Birth
A common area of misunderstanding for prospective parents concerns the success of the gender selection process. The research draws a clear distinction between the accuracy of gender identification and the overall success rate of a live birth.
The accuracy of PGT in determining an embryo’s sex is remarkably high, offering a success rate of over 99%. This means that once a specific embryo is selected, the chance of a technical error misidentifying its gender is exceptionally low. This is a critical point for managing patient expectations: while the choice of gender is virtually certain, the final outcome of a live birth is not. The successful transfer and implantation of an embryo—and its subsequent development into a healthy baby—remain contingent on numerous other factors, most notably the prospective mother’s age and overall health, embryo quality, and uterine health. For example, sample success rates for live birth at one clinic show a significant decline with age, from a 77% success rate for women in their 20s to only 25% for women in their 40s. This fundamental difference highlights that while the science of gender identification is mature, the overall process of achieving a live birth is still subject to the complexities of human biology.
The following table provides a clear comparison of the two primary forms of PGT:
| Test Name | Primary Purpose | Common Conditions Identified | Gender Selection Capability |
| PGD | Screening for specific gene mutations | Cystic fibrosis, hemophilia, Huntington disease | Yes |
| PGS (PGT-A) | Screening for chromosomal abnormalities | Down syndrome, Edward syndrome, Turner syndrome | Yes |
The Driving Forces: Understanding the Motivations
Medical Imperatives: The Uncontroversial Use
Gender selection is widely accepted by the medical community when used to prevent the transmission of serious sex-linked genetic disorders. A number of conditions, such as hemophilia and Duchenne muscular dystrophy, are primarily carried on the X chromosome and disproportionately affect male offspring. In such cases, a couple at risk of passing on one of these conditions may choose to select a female embryo to prevent the birth of a child who would inherit the disease. Organizations such as the American Society for Reproductive Medicine (ASRM) have explicitly endorsed sex selection for these medical reasons, framing it as an essential component of a couple’s right to have a healthy child.
Elective Gender Selection: Family Balancing and Personal Preference
The most common reason for non-medical gender selection is a desire for “family balancing,” a term used when parents wish to have a child of a gender that is underrepresented in their family. For example, a family with several sons may decide to transfer a female embryo in their next cycle. This rationale is often intertwined with deeper personal and emotional factors. Some parents may feel more emotionally or psychologically prepared to raise a child of a particular gender. Others, particularly those who have experienced the loss of a child, may choose the gender of their next baby as part of a personal healing process. For couples already undergoing the physically and emotionally taxing process of IVF for infertility, the ability to choose the gender is sometimes seen as a welcome “perk” or a positive aspect of an otherwise challenging journey.
Cultural and Societal Influences
While family balancing may seem like a purely personal choice, the motivations behind it are often influenced by deeper cultural and societal factors. In many cultures, particularly in parts of Asia and Eastern Europe, a strong preference for male offspring exists due to practices like inheriting the family name or the expectation that sons will provide for their parents in old age. This societal pressure can lead families to seek gender selection services, even traveling abroad if the practice is prohibited in their home country.
The proliferation of gender selection technology, particularly when a societal bias for one sex exists, can have significant and long-lasting consequences. The practice of sex-selective abortion or embryo selection has resulted in a global imbalance in sex ratios, with an estimated 142 million women and girls “missing” worldwide. This gender imbalance has been linked to a number of severe socioeconomic problems, including an increase in sexual violence, human trafficking, and political unrest in the affected countries. This demonstrates that while the decision to select a child’s gender may be an individual one, the aggregate effect can perpetuate deeply rooted gender inequalities and have a negative impact on the collective social fabric.
The Global Perspective: Legal, Ethical, and Financial Considerations
The Legal and Regulatory Maze
The legal and regulatory landscape of elective gender selection is highly fragmented, with no unified global policy. This has created a patchwork of regulations that directly influences patient behavior and the rise of medical tourism.
- Strict Prohibitions: Many nations, including Australia, Canada, and the UK, have enacted laws that outright ban gender selection for non-medical reasons. In these countries, the procedure is only permissible to prevent the transmission of serious sex-linked genetic disorders.
- Permissive Environments: In contrast, a number of countries have adopted more liberal policies, allowing for elective gender selection, often for “family balancing”. This group includes popular medical tourism destinations such as Cyprus, Mexico, Albania, Thailand, and the United Arab Emirates. These nations combine advanced medical facilities with flexible local regulations, attracting a large number of international patients from more restrictive countries.
- The United States: The United States lacks a national policy on the matter. While no federal law explicitly prohibits elective gender selection, the legality and availability can vary by state and individual clinic policy, which can lead to confusion and uncertainty for prospective parents.
The legal fragmentation has a direct causal relationship with the medical tourism industry. A patient’s inability to access gender selection services in their home country due to legal restrictions directly creates a demand for services in a more permissive environment. This drives a significant number of couples to travel abroad, where the procedure is both legal and often significantly more affordable. One personal account details a couple’s journey from a disappointing experience at a clinic in Cyprus to a more successful one, underscoring the complexities and challenges of navigating this global marketplace.
A Detailed Financial Overview
The cost of IVF with gender selection is a major consideration for prospective parents. The financial commitment varies dramatically based on geographic location and clinic, turning the practice into a global economic market.
In the United States, the total cost for one cycle of IVF with gender selection typically ranges from $27,000 to $30,000, though some clinics may offer lower prices. This significant investment includes several key components:
- Base IVF Procedures: The core IVF cycle, including monitoring, egg retrieval, and embryo transfer, costs between $9,000 and $14,000.
- Medications: Ovarian stimulation medications can add an additional $3,000 to $7,000 to the total cost.
- Genetic Testing: PGT fees, which are essential for gender selection, range from $2,000 to $5,500.
- Additional Procedures: Other procedures like Intracytoplasmic Sperm Injection (ICSI) or cryopreservation and storage of embryos can incur further costs. Costs can also fluctuate based on the clinic’s location, with urban centers like New York City often having higher prices than rural areas.
The stark price disparity between the U.S. and popular medical tourism destinations is a powerful economic incentive for international travel. The following table provides a clear comparison of costs in major markets:
Cost of IVF Gender Selection: A Comparative Overview
| Country/Region | Legal Status for Elective Use | Estimated Total Cost (USD) |
| United States | Varies by State/Clinic | $27,000 – $30,000+ |
| Mexico | Generally Legal for Family Balancing | $5,000 – $7,000 |
| Cyprus | Legal for Non-Medical Reasons | $5,000 – $6,000 |
| Thailand | Legal for Medical and Non-Medical Reasons | $7,000 – $8,000 |
| United Arab Emirates | Legal for Family Balancing | $8,000 – $10,000 |
The Ethical Debate: Weighing Competing Values
The ethical debate surrounding elective gender selection is complex, as it pits an individual’s right to reproductive freedom against potential collective and societal harms.
Arguments Against the Practice
The primary arguments against elective gender selection are rooted in concerns about societal values and the direction of human reproduction. One of the most frequently cited concerns is the “slippery slope” argument. Critics contend that permitting gender selection will inevitably lead to parents seeking to select for other non-health-related traits, such as eye color, intelligence, or athletic ability, potentially ushering in a future of “designer babies”. Another major objection is the “instrumentalization” or commodification of embryos, where embryos are created specifically for the purpose of selection and those with “undesired” traits are discarded. This is seen as a violation of the sanctity of human life and a fundamental alteration of the parent-child relationship from one of unconditional love to one of fulfilling parental expectations.
Furthermore, gender selection is criticized for its potential to reinforce societal gender biases and promote a form of eugenics. The practice is seen as perpetuating the harmful idea that one gender is more valuable than another, a notion that is already prevalent in some cultures and contributes to gender inequality.
Arguments for the Practice
Proponents of elective gender selection focus on the principles of individual autonomy and reproductive freedom. They argue that individuals have a fundamental right to make decisions about their own families and reproductive journeys. A core argument is that allowing parents to achieve their desired family composition can lead to greater happiness and a more harmonious home environment. For couples who have experienced the loss of a child, the ability to choose the gender of a subsequent child can be an important part of the healing process. The ethical conflict at the heart of the debate is the tension between the freedom of an individual to pursue their personal reproductive choices and the potential for these choices, when scaled up, to have negative social consequences. This is a fundamental challenge that will likely continue to evolve as reproductive technologies advance.
Beyond PGT: Evaluating Alternative Methods
The Limitations of Non-IVF Methods
In the history of gender selection, a handful of alternative methods have been developed, though most have proven to be either unreliable or are no longer available. A notable example is the Microsort™ sperm-sorting technique, which attempted to separate X-bearing (female) and Y-bearing (male) sperm based on their DNA content. This method, which was used in conjunction with intrauterine insemination (IUI) or IVF, was reported to have a lower accuracy rate, approximately 90% for girls and 85% for boys, compared to PGT. After an extended review period, the U.S. Food and Drug Administration (FDA) did not grant approval for Microsort™ to be used clinically, and the technique is no longer available in the United States. The fact that this once-promising alternative is now off the market solidifies PGT as the only reliable, medically sanctioned method for gender selection.
Low-Tech Approaches: Myths and Realities
Beyond the clinical realm, a variety of low-tech, at-home methods for gender selection have been popularized, but they lack any scientific basis. The most well-known is the Shettles method, which theorizes that a couple can influence a child’s sex by timing intercourse in relation to ovulation, using specific sex positions, or altering the vaginal environment. Proponents of this method claim success rates as high as 75-80%, but this is not supported by independent research. Experts agree that such methods are no more reliable than the natural 50/50 odds of conceiving a boy or a girl. Other folk wisdom, such as specific dietary changes, is also not supported by any scientific evidence. While harmless to attempt, these methods offer no real influence over the outcome.
The following table provides a definitive summary of the various methods for gender selection.
Methods for Gender Selection: An Overview
| Method | Scientific Basis | Accuracy | Status |
| PGT/IVF | High (based on chromosomal analysis) | >99% | Widely available (in permissive countries) |
| Sperm Sorting (MicroSort™) | Medium (based on DNA content) | 85−90% | Discontinued for clinical use in the U.S. |
| Shettles Method | None (based on folk wisdom/unproven theories) | 50/50 | Unproven/Folk Method |
Conclusion and Guidance
A Framework for Informed Decision-Making
Gender selection through IVF is a deeply personal and often complex decision that requires careful consideration of scientific, financial, legal, and ethical factors. The report’s analysis confirms that Preimplantation Genetic Testing (PGT) is the only reliable and accurate method for gender selection, offering nearly 100% certainty in identifying the sex of an embryo. This technology is a powerful tool, providing a medical solution for couples at risk of passing on sex-linked genetic diseases and offering a path for family balancing to others.
However, the practice is not without its challenges. The significant financial cost, particularly in the United States, and the fragmented global legal landscape compel many to travel abroad, creating an international market that can be difficult for patients to navigate. The ethical debate, which raises profound questions about the sanctity of life, the potential for eugenics, and the societal implications of gender preference, is ongoing and provides a critical framework for personal reflection.
Prospective parents considering this option are advised to engage in a thorough consultation with a qualified fertility specialist and genetic counselor to fully understand the clinical process, risks, and potential outcomes. Equally important is a personal and open-minded assessment of their motivations and the ethical considerations involved.
Future Directions: The Evolution of Reproductive Technology
The field of reproductive technology continues to advance rapidly. While PGT offers a powerful tool for screening, emerging technologies such as polygenic screening could expand the scope of genetic selection beyond single genes and chromosomal abnormalities to include complex traits with a polygenic basis, such as heart disease or intelligence. These advancements will undoubtedly intensify the ethical debate and further test the boundaries of what is considered acceptable in reproductive medicine. As technology progresses, it becomes increasingly imperative for legal and ethical frameworks to keep pace, ensuring that reproductive choices are made responsibly and with a full understanding of their potential impact on both the individual and society as a whole.
IVF Gender Selection with Cure Holiday
Family completion or family balancing is one of the biggest dreams of many couples. At Cure Holiday, we are here to guide you on this special journey and safely turn this dream into a reality. Through our modern and high-tech clinic partners in Turkey and Cyprus, we offer the most up-to-date in vitro fertilization (IVF) treatments combined with the option of gender selection.
Our Process: Trust and Technology Combined
Gender selection is performed using preimplantation genetic testing (PGT), an integral part of the IVF process. Thanks to this advanced technology:
- Genetic Analysis: The created embryos are examined in detail not only for their gender (XX or XY) but also for possible genetic abnormalities. This maximizes your chances of a healthy pregnancy.
- Up to 99% Accuracy: PGT testing offers almost complete accuracy in determining the embryos of the gender you wish to select.
- Safe and Ethical Approach: All our treatment processes are carried out in meticulous compliance with international legal and ethical standards.
Why Turkey and Cyprus?
Turkey and Cyprus stand out as global IVF centers due to their high success rates and experienced health professionals. While offering the best treatment to our patients, we also make the process much more accessible with competitive prices.
Why Cure Holiday?
At Cure Holiday, we combine these advantages with a special and personal experience for you. When you work with us:
- Expert Physicians: You work with trusted doctors who are specialists in their fields and have international experience.
- Personalized Service: We focus on the unique needs of each of our patients to create the most suitable and personalized treatment plan for you.
- Affordable Prices: Without compromising on quality, we offer budget-friendly and transparent pricing.
At Cure Holiday, our goal is not just to provide a treatment but also to support you throughout this sensitive process. Contact us to get one step closer to your dream family in a comfortable and safe environment.