What Is Gender Selection And How Is It Performed?
Gender selection is the process of genetically examining embryos created during in vitro fertilization (IVF) treatment to determine the desired gender before transferring them to the uterus. The process primarily involves taking a small sample of cells from the embryos on Day 5 or Day 6, a procedure known as a biopsy.
Subsequently, in the genetic laboratory, the embryo’s sex chromosomes (XX or XY) are analyzed. Only the embryos that are confirmed to be genetically healthy and of the desired gender are selected for transfer. This method serves a vital role for family balancing purposes and is medically critical for preventing the transmission of X-linked genetic diseases.
What Legal Restrictions Apply In Which Countries?
Legal regulations regarding gender selection practices differ significantly from one country to another. In Turkey and many European Union countries, this procedure is only legally permissible in cases of medical necessity (to prevent sex-linked genetic disorders).
However, in destinations like Cyprus and Thailand, it is legally allowed for the purpose of family balancing. Before starting treatment, it is critically important to thoroughly understand the current legislation and ethical guidelines of your chosen country to avoid legal issues and ensure a smooth treatment process. You can obtain the most current legal and ethical information on this matter by seeking support from Cure Holiday experts.
Who Are The Most Suitable Candidates For Gender Selection?
The most suitable candidates for gender selection treatment are generally younger couples who have sufficient ovarian reserve and a high potential to yield a significant number of healthy embryos from the IVF procedure. Furthermore, couples who already have one or more children and seek a child of the opposite sex for family balancing purposes form the primary candidate group.
However, this treatment is also appropriate for couples who need to choose a specific gender due to a medical necessity to avoid the risk of passing on a serious genetic disease (such as hemophilia). In every case, a detailed health screening and genetic counseling process are mandatory prerequisites.
What Is The Difference Between PGT-A And Gender Selection?
PGT-A (Preimplantation Genetic Screening – Aneuploidy) is a test performed to check if the embryo has a normal number of chromosomes (a healthy 46 chromosomes), and its primary goal is to increase the chance of pregnancy and prevent miscarriage. Gender selection is the determination of the embryo’s X and Y chromosomes as part of this PGT-A screening. Essentially, gender information is an output provided by the PGT-A test. For a successful gender selection transfer, the transferred embryos must not only be of the desired gender but also have a normal PGT-A result, which maximizes the overall success rate of the procedure.
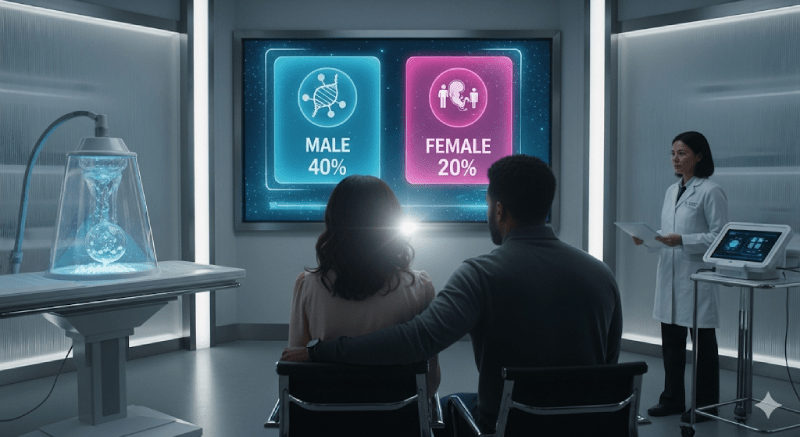
How Do Success Rates Change According To Age?
The success rate of gender selection, fundamentally being an IVF treatment, changes significantly depending on the woman’s age and, consequently, the quality of her eggs. In women under 35 years old, the chance of obtaining suitable healthy embryos for PGT is higher due to the greater number and quality of eggs retrieved. As age advances, particularly after 40, the rate of finding healthy embryos suitable for gender selection decreases because the risk of chromosomal abnormalities in the eggs increases. Therefore, treatments started at a younger age generally yield more successful outcomes in terms of both cost-effectiveness and reduced emotional strain.
What Tests Are Required Before Starting Treatment?
Standard IVF preparation tests are required before starting gender selection treatment. For the woman, hormone analyses are requested, including AMH (Anti-Müllerian Hormone) levels, FSH, LH, E2, infection screenings, and an ultrasound to assess the uterine structure. For the man, a detailed sperm analysis is requested to determine the quality, count, and motility of the sperm. These tests are mandatory for determining the dosages and timing of the ovarian stimulation protocol to be applied, and for predicting the potential success of the treatment. It is also required that all records related to your medical history are complete and up-to-date.

How Is The Sperm Preparation And Washing Process Done?
The sperm sample is collected in a private room at the clinic on the day of egg retrieval and is then subjected to a washing and preparation procedure in the laboratory. The goal of this process is to clean out dead cells, infection residues, and immobile sperm from the sample, thereby concentrating the healthiest, most motile, and morphologically best sperm. This highly concentrated and quality sperm sample is then used to fertilize the collected eggs using the ICSI (Intracytoplasmic Sperm Injection) technique. This preparation step is a critical laboratory action that directly increases the chances of successful fertilization.
Is The Egg Retrieval Process Painful?
The egg retrieval procedure is performed under light sedation or general anesthesia for the patient’s comfort and typically takes 20 to 30 minutes. Therefore, the patient does not feel any pain or discomfort during the procedure itself. The procedure is performed vaginally using a fine needle guided by ultrasound. Following the procedure, mild abdominal cramps or a feeling of fullness are considered normal and can usually be easily managed with simple pain relievers. Patients are generally discharged on the same day after a short recovery period. This level of comfort is a critical indicator of treatment quality at internationally accredited clinics.
On Which Day Is The Embryo Biopsy Performed?
The embryo biopsy, for the purpose of obtaining genetic material for gender selection, is performed at an advanced stage of the embryo’s development. The most ideal time is when the embryo has reached the blastocyst stage on Day 5 or Day 6. At this stage, a few cells are carefully taken from the outer layer of the embryo (the trophectoderm). This timing ensures that the amount of cells taken is sufficient for analysis and minimizes the risk of damage to the inner cell mass of the embryo (the part that will form the baby). This must be performed meticulously by an experienced embryologist using specialized equipment.
Does The Biopsy Harm The Embryo?
When performed by experienced laboratories and skilled embryologists at the blastocyst stage (Day 5 or Day 6), the risk of the embryo biopsy causing permanent harm to the embryo is extremely low. Since the cells are taken from the part of the embryo that will form the placenta and outer membrane (trophectoderm), the inner cell mass that will form the baby itself is not directly touched. Thanks to modern techniques and rapid freezing-thawing (vitrification) methods, the embryos’ survival rates remain above 90%. This minimal risk is outweighed by the high chance of success offered by transferring a healthy and genetically tested embryo.
How Long Do PGT Results Take To Come Back?
After the embryo biopsy is performed, the analysis of the genetic material and the results reaching the clinic typically take between 10 and 14 days. During this period, all biopsied embryos are safely kept frozen (vitrified) until the results are returned. The embryo, having completed the genetic analysis, is thawed and transferred in a subsequent menstrual cycle after it is confirmed to be genetically normal and of the desired gender. The speed of receiving results may vary slightly depending on whether an external laboratory is used for analysis and the current volume of genetic testing.
What Are The Failure Rates In Gender Selection?
The failure rate in gender selection is associated not directly with the selection itself, but rather with the health status of the embryo and its ability to implant in the uterus. The chance of achieving pregnancy with a single healthy, PGT-A-screened blastocyst is generally between 50% and 70%. Failure occurs when the embryo fails to implant (implantation failure) or when no healthy embryos of the desired gender are found during the genetic analysis. To minimize these probabilities, the quality of the egg and sperm retrieval process, combined with laboratory quality, are critically important factors for the final outcome.
When Is Frozen Embryo Transfer Performed?
Frozen Embryo Transfer (FET) is performed in the next menstrual cycle after the 10−14 day waiting period for PGT results, once the embryo’s genetic status is confirmed. The purpose of this transfer is to create a uterine environment that is free from the effects of ovarian stimulation medications, hormonally optimized to ideal levels, and possessing high receptivity. Once the uterine lining thickness and appearance are confirmed to be ideal (generally above 7 mm), the transfer is carried out. FET is often the preferred method in many clinics because it sometimes offers higher pregnancy rates than a fresh transfer.
How Is The Uterus Prepared Before Transfer?
Before a frozen embryo transfer, the uterus is carefully prepared, typically using estrogen and progesterone hormone supplements. Estrogen promotes the thickening of the uterine lining (endometrium) to reach the ideal 7−14 mm thickness. This process is closely monitored through ultrasound and blood tests. Once the uterine lining reaches the appropriate thickness, progesterone hormone is added to open the “implantation window,” making the lining ready to accept the embryo. This preparation can be performed using a natural cycle or a medically controlled cycle and is designed to maximize the embryo’s chance of successful attachment.
What Hormone Medications Are Used During Treatment?
Since gender selection treatment includes a standard IVF protocol, Gonadotropin medications containing FSH and LH are initially used to stimulate the ovaries. These medications aim to develop multiple follicles simultaneously. GnRH agonists or antagonists are also included in the treatment protocol to prevent premature ovulation. When the eggs are mature, HCG (the trigger shot) is administered to induce final maturation. Following the transfer, progesterone supplements (in the form of suppositories, gel, or injections) are invariably prescribed to support the uterine lining and facilitate implantation during the critical waiting period.
What Does The Total Cost Of Treatment Consist Of?
The total cost of gender selection treatment is higher than that of a standard IVF treatment, and the main components are: the Basic IVF package (including egg retrieval, fertilization, and culturing), the PGT-A Genetic Screening fee (per embryo or package price), the cost of hormone medications (which varies with the stimulation dosage), embryo freezing and storage fees, and the cost of the Frozen Embryo Transfer (FET) procedure. For international treatments, travel, accommodation, and interpreter costs must also be factored into the total budget. For a transparent and current cost breakdown, you should seek assistance from Cure Holiday.

Why Is Gender Selection Popular In Cyprus?
Cyprus enjoys significant popularity among international patients because gender selection for family balancing purposes is legally permitted within specific regulations. The island is distinguished by its geographical proximity, easy accessibility, and centers that maintain high medical standards. Clear legal processes, the use of advanced laboratory technologies, and the offering of generally cost-effective packages make Cyprus an attractive destination. Furthermore, the prevalence of Turkish-speaking medical staff and guidance services makes the treatment process more comfortable, especially for patients coming from Turkey and neighboring regions.
What Are The Gender Selection Possibilities In Thailand?
Thailand is a leading country in medical tourism in Asia, known for its technologically advanced, internationally accredited clinics. PGT-A is also used for gender selection in Thailand, although the legal framework and ethical approaches may differ from those in Cyprus. IVF Clinics in Thailand are recognized for their high laboratory quality, specialized staff, and superior patient care. This medical expertise, combined with the cultural appeal of the Far East, makes Thailand an alternative international destination for gender selection. Cure Holiday expertise can assist you in planning your travel and accommodation logistics for treatment in Thailand.
How Should International Travel Be Planned For Treatment?
International travel for gender selection treatment must be meticulously planned according to the treatment schedule. Ovarian stimulation can generally be started in your home country, but you will need to stay in the chosen country for approximately 10 to 14 days for egg retrieval, biopsy, and transfer (FET). Flights should be arranged with caution, particularly considering the necessity of avoiding heavy exertion after the transfer procedure. Your accommodation should be close to the clinic due to frequent appointments. Making a flexible travel plan with contingency allowances for unexpected delays will help reduce stress. Cure Holiday plans the most suitable logistics on your behalf during this complex process.
How Are Accommodation And Transportation Issues Resolved?
Accommodation and transportation in international treatments directly influence the comfort and success of the procedure. It is recommended to choose comfortable accommodation options that are quiet and conducive to rest, located near the clinic. Since you will need to travel to the center frequently during the treatment process, ease of transportation is critically important. Cure Holiday can arrange apartments or hotels close to the treatment center that fit your budget and coordinate transportation between the clinic and your accommodation. This way, patients can fully focus on their treatment instead of dealing with logistical details.
What Are The Side Effects Of Gender Selection Treatment?
Since gender selection treatment involves an IVF cycle, the side effects are the same as standard IVF side effects. These include slight pain or bruising at the injection site, abdominal bloating and tenderness, mood swings, and feelings of fatigue. The most serious but rare risk is the development of OHSS (Ovarian Hyperstimulation Syndrome). Since the embryos are frozen for PGT (meaning FET is performed), the risk of severe OHSS is reduced. Hormone levels are closely monitored to minimize these risks. Immediate contact with the clinic is required should any severe side effects occur during the stimulation phase or afterwards.
Is Sexual Intercourse Allowed During The Process?
It is crucial to be cautious regarding sexual intercourse during the different stages of the treatment process and to strictly follow the doctor’s instructions. During ovarian stimulation, sexual intercourse may be restricted to prevent discomfort due to enlarged ovaries and to avoid the rare risk of ovarian torsion. Following egg retrieval and especially during the waiting period after frozen embryo transfer, sexual abstinence may be advised to prevent pressure on the uterus and reduce the risk of infection. These restrictions are temporary and important precautions necessary to ensure the success of the treatment.
How Should Nutrition Be Managed During Treatment?
Nutrition during treatment is vital for supporting egg and embryo quality and maintaining overall health. A Mediterranean-style diet (rich in vegetables, fruits, whole grains, and healthy fats) is recommended. Processed foods, excessive sugar, alcohol, and caffeine should be strictly avoided. The regular use of vitamin and antioxidant supplements recommended by the doctor, especially folic acid, is important. Adequate water consumption can help lower the risk of OHSS, particularly during the stimulation period. A healthy diet positively influences both the ovarian response and the receptivity of the uterine lining.
What Are The Alternatives In Case Of Recurrent Failure?
In cases of recurrent failure in gender selection attempts (especially implantation failure), the treatment approach must be re-evaluated and changed. Alternatives include performing the ERA (Endometrial Receptivity Array) test to check uterine lining receptivity, investigating and adding treatments for immunological factors (such as intralipid infusion), trying different stimulation protocols, or using advanced laboratory techniques like IMSI to enhance sperm quality. Thoroughly investigating the cause of the failure and personalizing the treatment protocol are critical steps that will lead to success in the next attempt.
What Is The Connection Between PGT-M And Gender Selection?
PGT-M (Preimplantation Genetic Diagnosis – Monogenic) is performed to detect serious hereditary diseases caused by a single gene defect (such as cystic fibrosis) in the embryo. If the disease occurs only in a specific sex (e.g., X-linked inheritance), gender selection is obligatorily performed alongside PGT-M. In this scenario, gender selection is a treatment step driven by medical necessity, and this practice is legally supported in many countries. Gender selection plays a vital role in preventing the transmission of such genetic diseases to future generations.
How Many Embryos Are Recommended For Transfer?
Since PGT-A screening is performed in gender selection treatment, the transferred embryos are known to be genetically normal. This inherently increases the chance of implantation. Therefore, to minimize the risk of multiple pregnancies, the transfer of only a single embryo (SET) is strongly recommended. Single embryo transfer significantly reduces the possibility of twin or triplet pregnancies, which can be risky for both the mother and the babies, while maintaining high success rates. The decision on the number of transfers is made by the doctor and the ethics committee, considering the patient’s age and previous transfer history.
How Is The Risk Of Multiple Pregnancy Reduced?
The most effective way to reduce the risk of multiple pregnancy, as mentioned above, is the transfer of only a single embryo (SET) that has been proven to be of high quality through genetic screening. Single transfer dramatically reduces the risk of multiple pregnancies, especially in younger patients with optimal uterine receptivity. Since multiple pregnancies increase the risk of complications like premature birth, low birth weight, and preeclampsia in the mother, modern IVF approaches strongly advocate for single embryo transfer. You can inquire about current clinic policies on this matter through Cure Holiday.
When Is Psychological Support Needed In Treatment?
The gender selection process can create intense psychological pressure due to both the physical and emotional burden of IVF treatment and the expectation of a specific gender. If continuous anxiety, stress, sleep disorders, or depressive feelings are experienced during this process, seeking professional support is necessary. Psychological support helps increase emotional resilience, develop coping mechanisms for stress, and maintain adherence to the treatment plan. Treatment centers generally provide access to such support services. You can evaluate the counseling services provided by Cure Holiday to manage your emotional journey.
What Factors Increase Success In Gender Selection Treatment?
The most important factors that increase success in gender selection treatment are the woman’s young age and the resulting high egg quality (which increases the number of healthy embryos), the quality of the laboratory utilized (expertise in biopsy and freezing-thawing), and the optimal receptivity of the uterine lining. Furthermore, the couple’s maintenance of a healthy lifestyle, avoiding smoking and alcohol, also supports success. Eliminating potential risk factors through detailed medical analysis before treatment and personalizing the treatment protocol according to these factors form the foundation of success.
What Are The Legal Documents And Approval Processes Like?
When undergoing gender selection treatment abroad, the legal and ethical approval processes are extremely important. Couples are required to submit a series of legal documents, such as marriage certificates, identification documents, and sometimes notarized consent forms, in compliance with the laws of the country where the treatment will be placed. Before commencing treatment, an approval certificate for gender selection may need to be obtained from the clinics’ ethics committees. Cure Holiday provides full support in the preparation, translation, and submission of these documents in compliance with legal formats, thereby alleviating the bureaucratic burden.
Is The Use Of Donor Sperm Or Eggs Possible?
Gender selection treatment can also be performed using donor sperm or eggs, provided that suitable genetic material is secured. This becomes a necessity, especially in cases where the woman’s ovarian reserve is depleted (egg donation) or where the man has severe sperm problems (sperm donation). When donor material is used, the resulting embryos are still screened with PGT-A, and a healthy embryo of the desired gender is transferred. Donor selection and this process’s legal requirements must be carried out meticulously according to the laws of the chosen country.
What Happens To Unhealthy Embryos After PGT?
The fate of embryos found to be genetically abnormal after PGT (Preimplantation Genetic Diagnosis), or healthy embryos of the undesired sex, is determined by the selected clinic’s ethical rules and the country’s legal regulations. Generally, couples are offered options such as destruction of these embryos, donation for medical research, or continued storage at the clinic. This is a sensitive process determined by the ethical and conscientious decisions of the couples, and clinics are obliged to respect these decisions. Cure Holiday can help you access ethical counseling during this process.
What Is The Total Timeframe For The Treatment Process?
The total timeframe for gender selection treatment, from the initial consultation to the pregnancy test, generally spans between 6 and 8 weeks. This duration includes stimulation (10−14 days), biopsy, waiting for genetic results (10−14 days), and the preparation period for frozen embryo transfer. The overall treatment duration may extend due to the waiting period for results, but the most intensive part is the 10−14 day travel period spent abroad. When planning, you should consider this total timeframe and allow for flexibility.
What Should Be Considered When Choosing A Clinic?
The considerations when choosing a clinic are not limited to just whether gender selection is legal. The clinic’s up-to-date laboratory technology (expertise in vitrification and biopsy), embryologist experience, live birth success rates per transfer, transparent pricing policy, and competence in international patient management are all important factors. Additionally, the quality of the logistical support and interpreter services offered by the clinic is a determinant of your comfort. Consulting Cure Holiday is recommended for detailed comparisons of high-standard clinics that meet these crucial criteria.
How Does Cure Holiday Provide Support?
Cure Holiday offers comprehensive guidance and organization services from A to Z for couples planning to undergo gender selection treatment. Support services include: identifying and comparing reliable clinics where the procedure is legally permitted, obtaining the most suitable price quotes, translating and transferring medical records to the clinic, organizing all travel, accommodation, and transportation logistics, and providing 24/7 local guidance and interpretation services at every stage of the treatment. Cure Holiday manages all complex processes, minimizing the stress for couples so they can focus entirely on their treatment.
How Long Should Medications Be Used After Transfer?
Supportive hormone medications, such as progesterone and estrogen, used after embryo transfer, must be continued for a period even after the pregnancy test returns positive. These medications are vital for supporting the pregnancy in its early stages and strengthening implantation. Generally, supportive medications are gradually reduced and discontinued between Week 8 and Week 12 of pregnancy. Your doctor will determine the dosage and exact time to stop these medications based on the results of your blood hormone tests. Stopping the medications without doctor approval can increase the risk of miscarriage, so instructions must be strictly followed.