What Is The Most Common First Symptom Of Lung Cancer?
The most common first symptom of lung cancer is especially a persistent, nagging cough that lasts longer than two weeks and does not go away. Although this is often attributed to smoking by smokers, any change in the character of the cough (such as worsening or a difference in sound) must be taken into account. Other important symptoms include shortness of breath, especially with exertion, coughing up blood (hemoptysis), persistent pain in the chest or shoulder area, and unexplained weight loss. If any of these symptoms are noticed, it is necessary to consult a specialist immediately to avoid missing the opportunity for early diagnosis.
What Diagnostic Method Is Used For A Persistent Cough?
The initial diagnostic method used for a persistent and unexplained cough is generally a chest X-ray, but a low-dose computed tomography (CT) scan is essential for detailed examination. While X-rays can show large masses, a CT scan has the ability to detect much smaller, early-stage nodules, especially in high-risk individuals with a history of smoking. Even if the cough is not caused by cancer, a CT scan provides detailed information about other potential problems in the lung (infection, emphysema), and the next steps for definitive diagnosis (PET-CT or biopsy) are planned accordingly.
What Are The Main Risk Factors For Lung Cancer?
The main risk factors for lung cancer primarily include smoking and tobacco product use. The risk is dramatically higher in smokers compared to non-smokers. However, risk factors are not limited only to smoking. The second significant risk is exposure to smoke (passive smoking) and certain occupational exposures. Exposure to chemicals like asbestos, radon gas, and chromium increases the risk. Additionally, a family history of lung cancer and previous severe lung diseases (COPD, fibrosis) also cause the risk to increase due to genetic predisposition.
Why Is Computed Tomography (CT) Scanning Vital?
Computed Tomography (CT) scanning, especially the method known as low-dose CT screening, is vital for the early diagnosis of lung cancer. It can detect nodules even before symptoms appear or when the tumor is very small, particularly in high-risk individuals (those who have smoked heavily or continue to do so). Cancer caught in the early stages greatly increases the chance of complete cure with surgery. This screening is regularly recommended for heavy smokers between the ages of 55 and 74 and has been proven to reduce cancer-related deaths.
What Is The Purpose Of PET-CT Scanning In The Diagnostic Process?
PET-CT (Positron Emission Tomography – Computed Tomography) scanning is used in the diagnostic process to determine whether the mass or suspicious nodules are cancerous and, if so, where the cancer has spread in the body (staging). PET shows areas where cancer cells are metabolically active (glucose consumption), while CT provides the anatomical location of these areas. This combined imaging is extremely sensitive in detecting the location of the cancer, its spread to lymph nodes, and whether it has metastasized to distant organs. Accurate staging is fundamental for selecting the most appropriate treatment plan (surgery, radiotherapy, or systemic therapy).
What Types Of Biopsy Are Used To Make A Definitive Diagnosis?
The types of biopsy used to make a definitive diagnosis in lung cancer vary depending on the location and size of the mass. The most common methods used are Needle Biopsy (guided through the skin using CT or ultrasound), Bronchoscopic Biopsy (inserted through the airways), and Endobronchial Ultrasound (EBUS) Biopsy (to take samples from lymph nodes around the airways). The tissue sample obtained through biopsy not only confirms the presence of cancer but also determines the type of cancer and its genetic characteristics, paving the way for personalized treatment.
What Is The Importance Of Staging In Lung Cancer?
Staging in lung cancer determines how far the disease has spread (tumor size, spread to lymph nodes, and distant organ metastasis) and forms the basis of the treatment plan. In early stages (Stage I-II), the goal is usually surgery for a complete cure. In locally advanced stages (Stage III), treatment is a combination of chemoradiation. In the metastatic stage (Stage IV), treatment shifts to systemic therapies such as immunotherapy and smart drugs, focused on prolonging the patient’s quality of life. Accurate staging is a critical step to prevent unnecessary or insufficient treatment.
What Is The Difference Between Small Cell And Non-Small Cell Cancer?
Lung cancer is divided into two main types: Small Cell Lung Cancer (SCLC) and Non-Small Cell Lung Cancer (NSCLC). SCLC, although less common, is an aggressive type that grows very fast and spreads early (metastasizes). Its treatment generally consists of chemotherapy and radiotherapy, with surgery rarely applied. NSCLC is more common, progresses slower, and is often treated with surgery in the early stages. NSCLC treatment can be personalized with targeted smart drugs based on genetic mutation analysis.
In Which Stages Is Surgical Treatment (VATS) Applied?
Surgical treatment is generally applied in early-stage (Stage I and II) Non-Small Cell Lung Cancers (NSCLC) and is the primary treatment method offering a chance for complete cure. Modern surgical techniques include Video-Assisted Thoracoscopic Surgery (VATS) and robotic surgery. Since VATS is performed through small incisions in the chest wall instead of a large cut, it provides the patient with the advantages of less pain, shorter hospital stay, and faster recovery. Even some Stage III patients may become candidates for surgery if the tumor shrinks after systemic treatment.
What Is The Role And Side Effects Of Chemotherapy In Lung Cancer?
Chemotherapy is a systemic treatment method that uses drugs to kill cancer cells. It is commonly used in both Small Cell and Non-Small Cell cancers. In early stages, it can be applied to shrink the tumor before surgery (neoadjuvant) or to reduce the risk of recurrence after surgery (adjuvant). In advanced stages, it is one of the main treatment options. Its side effects include fatigue, nausea/vomiting, hair loss, a weakened immune system, and nerve damage. Modern supportive treatments have made most of these side effects manageable.
For What Purposes And How Is Radiotherapy Applied?
Radiotherapy aims to destroy cancer cells using high-energy beams. The treatment is applied for both curative (healing) and palliative (symptom relief) purposes. Curatively, it can be used as SBRT (Stereotactic Body Radiotherapy) in early-stage patients who are not suitable for surgery. In locally advanced stages, its simultaneous application with chemotherapy (chemoradiation) is standard. Palliatively, it plays a vital role in controlling pain caused by cancer, bone metastases, or brain metastases. Modern techniques minimize damage to healthy tissue.
How Does Immunotherapy Treat Lung Cancer?
Immunotherapy is a revolutionary treatment method that activates the body’s own immune system to recognize and destroy cancer cells. Cancer cells use “checkpoints” (most commonly PD-L1/PD-1) to turn off the immune system; immunotherapy releases these checkpoints, allowing immune cells to attack the cancer. It is frequently used as the first option or in combination with chemotherapy in the treatment of metastatic NSCLC. Especially in patients with high PD-L1 expression, it can provide longer and more durable responses compared to chemotherapy.
When Is Smart Drug Treatment (Targeted Therapy) Applied?
Smart drug treatment is applied only to NSCLC patients in whom a specific genetic mutation (e.g., EGFR, ALK, ROS1) is detected in the tumor. These drugs attack these targets that are essential for the cancer cell’s growth and proliferation. They can have fewer side effects than standard chemotherapy and generally show much higher response rates. Before starting treatment, the presence of these genetic mutations must be confirmed in the patient’s biopsy or blood sample, meaning molecular testing is mandatory.
How Does Treatment Change When Resistance To Smart Drugs Develops?
The development of resistance to smart drugs after some time is an expected situation due to the genetic adaptation of cancer cells. The first step taken when resistance develops is to analyze new (secondary) mutations with a new biopsy or liquid biopsy. Based on these new mutations, a switch to second or third-generation smart drugs may be made. If the mutation is not suitable or the resistance mechanism is complex, the treatment strategy may revert to combinations of immunotherapy or chemotherapy.
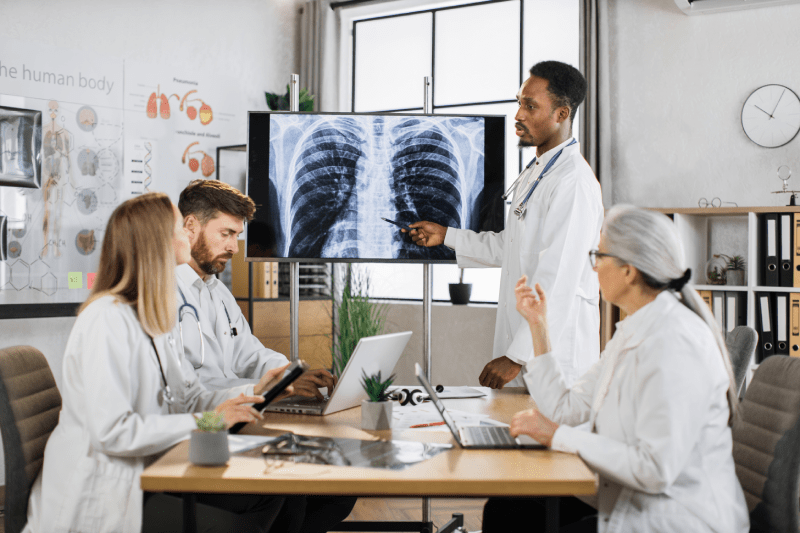
What Is The Importance Of A Multidisciplinary Approach In Lung Cancer?
A multidisciplinary approach in lung cancer means that the treatment plan is determined by an oncology board. This board brings together physicians from different specialties, such as a medical oncologist, radiation oncologist, thoracic surgeon, pathologist, and radiologist. This teamwork ensures the best possible evaluation of the patient’s tumor characteristics, stage, genetic structure, and general health status. This way, the patient has the chance to receive the most effective, personalized treatment combination based on current scientific data, which increases treatment success.
Which Molecular Tests Should Be Performed Before Treatment?
Molecular tests, which are vitally important before NSCLC treatment, map the genetic structure of the tumor. The main mutations examined are EGFR, ALK, ROS1, PD-L1 expression, and rarer genetic changes like BRAF and MET. These tests definitively determine whether the patient will respond to immunotherapy or which group of smart drugs. When tissue biopsy is insufficient or resistance develops, liquid biopsy performed from the blood can also be used as an alternative method for these tests.
How Is The Treatment Of Metastatic Lung Cancer?
The treatment of metastatic (Stage IV) lung cancer focuses on controlling the disease and improving the quality of life. Treatment is generally done with systemic methods (treatments that reach all parts of the body): Targeted smart drugs (depending on the mutation), immunotherapy (depending on the PD-L1 status), or chemotherapy if resistance develops to these treatments. If metastasis is only in one or a few areas (oligometastatic disease), long-term control may be aimed at by applying local radiotherapy (SBRT) to the spread area (brain, bone).
How Long Is The Recovery Period After Surgery?
The recovery period after surgery depends on the surgical technique applied (VATS/Robotic or open surgery) and the amount of lung tissue removed. In minimally invasive surgeries performed with the VATS method, the hospital stay is generally 3-7 days. Patients can return to light daily activities within 2-4 weeks. However, full recovery and return to intense physical activities, such as heavy lifting, can usually take 6 to 8 weeks. Breathing exercises and pain management are of great importance during the recovery process.
What Is The Importance Of Quitting Smoking During Treatment?
Quitting smoking during treatment is the most important and vital step in the fight against cancer. Smoking reduces the effectiveness of chemotherapy and radiotherapy, increases the severity of side effects, and slows down wound healing after surgery. Patients who quit smoking have a better response to treatment, experience milder side effects, and have longer overall survival times. Therefore, starting smoking cessation programs immediately upon diagnosis and completely ending this habit is essential.
How Should Nutrition Be Monitored During Treatment?
Good nutrition during treatment is critical for increasing the patient’s tolerance to treatment, preserving muscle mass, and strengthening the immune system. Since chemotherapy and radiotherapy can cause loss of appetite and nausea, small and frequent meals should be preferred. Focus should be on adequate protein and calorie intake. A balanced diet consisting especially of fresh fruits, vegetables, whole grains, and lean protein sources is important. Personalizing the nutrition plan according to side effects with the support of a dietitian preserves the patient’s overall condition.
How Many Sessions Does Immunotherapy Treatment Last?
Immunotherapy treatment for lung cancer generally requires a long-term treatment protocol lasting up to two years, but this duration may vary depending on the patient’s response to treatment and the doctor’s decision. Treatments are usually administered intravenously, at intervals of two, three, or four weeks. If the patient responds well to the medication and does not develop severe side effects, the treatment is continued. Unlike chemotherapy, immunotherapy aims to provide a long-lasting and more tolerable quality of life.
What Is Radiation Pneumonitis In Lung Cancer?
Radiation pneumonitis is an inflammatory reaction and damage that occurs in the lung tissue after irradiation in the area of radiotherapy. It usually occurs within 1 to 3 months after the end of radiotherapy and shows symptoms such as cough, fever, and shortness of breath. The severity depends on the dose of radiation and the area of the lung irradiated. Early diagnosis and management (usually with corticosteroids) are important to stop its progression. Modern radiotherapy planning techniques focus on sparing healthy lung tissue to minimize this risk.
Is Chemotherapy-Related Hair Loss Permanent?
No, chemotherapy-related hair loss, although varying depending on the type and dose of the drug used, is generally a temporary condition. Hair follicles become active again after chemotherapy ends. Hair usually begins to regrow within a few weeks or months after the end of treatment. The newly growing hair may initially have a different texture or color, but it returns to normal over time. During this process, the patient should receive psychological support and consider cosmetic solutions such as wigs, if necessary.
What Are The Costs Of Lung Cancer Treatment In Turkey?
Lung cancer treatment costs in Turkey are much more affordable and competitive compared to Western countries, especially in terms of access to high-cost treatments like immunotherapy and smart drugs. Turkey offers technological infrastructure and expertise at both US and EU standards, while general healthcare costs are significantly lower. The cost varies depending on the brand of the drugs used, the duration of hospital stay, and the specific treatment method applied (VATS, SBRT), but it provides a significant economic advantage for international patients.
How Is The Treatment Plan Adjusted According To The Patient’s Age?
The treatment plan is adjusted based on the patient’s biological age, general performance status, and coexisting diseases, rather than their chronological age. Elderly patients in good general health can receive the same standard treatments as younger patients. However, in elderly patients or those with additional diseases, chemotherapy doses may be reduced, or less intensive treatments (such as immunotherapy only) may be preferred to minimize side effects. The patient’s heart and lung reserves are carefully evaluated when deciding on surgery or intensive radiotherapy.
Does Lung Cancer Occur In Non-Smokers?
Yes, lung cancer can occur in non-smokers, accounting for about 10-25% of all cases. These cases are usually of the adenocarcinoma type. Although the cause is not fully known, factors such as exposure to radon gas, passive smoking, air pollution, family history of lung cancer, and previous severe lung diseases play a role. Since cancer in non-smoking patients usually has specific genetic mutations (like EGFR), it tends to respond very well to treatment with smart drugs.
To Which Patients Is SBRT (Stereotactic Body Radiotherapy) Applied?
SBRT is a high-precision radiotherapy method applied to patients, especially those with early-stage, small-sized lung cancer, who are too elderly or whose general health status is not suitable for surgery. In this method, a very high dose of radiation is concentrated on the tumor over a few days (usually 1 to 5 sessions). SBRT offers local control rates similar to surgery and allows for rapid recovery because it is minimally invasive.
How Is Fatigue Managed During The Treatment Process?
Fatigue (malaise) during the treatment process is one of the most common and challenging side effects caused by chemotherapy, radiotherapy, and the cancer itself. For its management, regular, low-intensity physical activity (brisk walking) is one of the most effective methods. Additionally, paying attention to good nutrition, sufficient sleep, and rest periods is important. Patients are advised to prioritize their daily tasks and accept help to conserve their energy. Medical conditions that may cause fatigue, such as anemia, should also be controlled.
What Is The Role Of Liquid Biopsy In The Diagnosis Of Lung Cancer?
Liquid biopsy is a method whose importance is increasing in diagnosis and treatment follow-up. As an alternative to tissue biopsy, it allows the analysis of circulating tumor DNA (ctDNA) released by cancer cells from a blood sample. Liquid biopsy offers a very fast and practical solution for determining genetic mutations non-invasively, monitoring the tumor, and especially for detecting new mutations when resistance develops to smart drugs.
Can Chemotherapy And Immunotherapy Be Applied Simultaneously?
Yes, chemotherapy and immunotherapy can be applied simultaneously (in combination) in the treatment of metastatic NSCLC (especially in patients with low PD-L1 expression). This combination allows chemotherapy to activate the immune system more effectively by using antigens released when it kills cancer cells. Studies have shown that this combined approach can provide higher and more durable response rates than chemotherapy or immunotherapy alone in some patient groups.
How Is The Risk Of Recurrence Followed Up After Treatment?
The risk of recurrence after treatment is managed by enrolling the patient in a regular and meticulous follow-up program. Follow-up is usually done at intervals of 3-6 months during the first two years, with physical examination, blood tests, and thorax/abdomen CT scans. PET-CT or brain MRI may also be included depending on the patient’s risk status. Since there is a risk of recurrence even in early stages, the patient’s symptoms and imaging results are carefully monitored. Early detection of recurrence increases the chance of successful salvage therapy.
Why Is Treatment Adherence And Discipline Very Important?
Treatment adherence and discipline are as important as technology and drugs in the success of lung cancer treatment. Timely delivery of chemotherapy or radiotherapy sessions, regular intake of smart drugs, and compliance with supportive treatment protocols (nutrition, exercise) are essential for the treatment to show maximum effectiveness. Non-compliance can lead to cancer cells developing resistance or the treatment not yielding the desired result. Approaching treatment with discipline is a factor that directly affects the patient’s survival.
How Do Chronic Diseases Affect Lung Cancer Treatment?
Chronic diseases such as diabetes, high blood pressure (hypertension), and especially cardiovascular diseases significantly affect lung cancer treatment. Chronic diseases reduce the patient’s tolerance to side effects related to surgery, chemotherapy, or radiotherapy. Treatment dosages and intensity may have to be adjusted according to the patient’s general health status. Therefore, chronic diseases should be controlled as best as possible before starting cancer treatment, and the treatment plan must be designed with a multidisciplinary approach that considers these existing conditions.
What Is The Role Of Palliative Care In Improving Quality Of Life?
Palliative care is a support system offered to every patient diagnosed with lung cancer, regardless of the disease stage, focusing on improving the quality of life. Its purpose is to control symptoms such as pain, shortness of breath, fatigue, and nausea resulting from cancer and its treatment, and to provide psychological, social, and spiritual support. Palliative care does not replace cancer treatment, but when applied concurrently with treatment, it improves the patient’s overall comfort, supports treatment adherence, and can even positively affect survival time.
What Technologies Are Used In Cancer Treatment In Turkey?
Oncology centers in Turkey utilize the most up-to-date technologies in lung cancer treatment. These include minimal invasive approaches in surgery such as VATS and Robotic Surgery; high-precision irradiation systems in radiotherapy that spare healthy tissue, such as IMRT, VMAT, and SBRT; PET-CT for diagnosis and staging; and advanced molecular pathology and genetic analysis laboratories for personalized treatment. This technological competence ensures a reliable and effective treatment environment for international patients.
Why Is Psychological Support Necessary During The Treatment Process?
The cancer diagnosis and challenging treatment process can cause intense emotional responses in patients, such as anxiety, depression, fear, and hopelessness. Therefore, receiving psychological support during the treatment process helps the patient cope with this emotional burden, maintain treatment adherence, and preserve their quality of life. Psycho-oncology specialists offer critical support for the patient and their family to become stronger on their cancer journey and develop stress management strategies.
What Are The Most Important Steps To Take To Prevent Lung Cancer?
The most important steps to take to prevent lung cancer are, as the primary and absolute priority, to quit smoking and avoid passive smoking. Secondly, it is important for individuals in the high-risk group (those with a history of heavy smoking) to participate in regular early detection screenings with low-dose CT scans as advised by a doctor. Other steps include a healthy and balanced diet, regular physical activity, avoiding exposure to environmental toxins (radon gas, asbestos) at home and work, and maintaining general health.
What Are The Advantages Of Receiving Lung Cancer Treatment In Turkey?
The biggest advantages of receiving lung cancer treatment in Turkey are that it offers high-quality medical services (internationally accredited hospitals) at much more affordable costs compared to Western countries. Patients can access the latest immunotherapy and smart drugs without long waiting times. Additionally, comprehensive health tourism services offered during the treatment process (translation, accommodation, transfer) and the ability for patients to relax with touristic activities after treatment make this process more comfortable.
How Does Lung Cancer Progress If Not Diagnosed Early?
If not diagnosed early, lung cancer progresses by first spreading to the lymph nodes within the lung and surrounding tissues, and then metastasizing via the bloodstream to distant organs (bone, brain, liver). This situation severely limits treatment options and the chance of a complete cure. In the advanced stage (Stage IV), treatment becomes more complex and usually focuses on controlling the disease and prolonging the patient’s lifespan. Therefore, taking symptoms seriously and not neglecting regular screenings are vital.
Lung cancer treatment is a complex process requiring a personalized and multidisciplinary approach. Access to accurate information and expertise at international standards is paramount during this process.
To evaluate the treatment plan best suited to your individual situation in Türkiye, access advanced oncology treatment centers, and receive professional health tourism support throughout the entire process, please contact Cure Holiday. We’re here to help you make the best decision for your health.