The Bariatric Imperative—A Strategic Perspective for Norwegian Patients
Obesity represents a growing health crisis in Norway and globally, creating significant challenges for Norwegian patients seeking bariatric surgery. The country’s healthcare system faces a dual challenge: prohibitive costs in the private sector and restrictive, bureaucratic processes within the public system. While Norway offers high-quality healthcare, access is severely limited by both financial and procedural constraints.
This situation compels patients to seek more accessible and comprehensive alternatives. In this context, Turkey has emerged not merely as a more affordable option but as a holistic solution known as a “Cure Holiday” that redefines the patient journey. This model transforms the traditional, fragmented approach to treatment by offering a seamless, high-quality, and highly accessible alternative.
The key findings reveal the complexity of the situation in Norway and the clear advantages of the Turkish solution. Patients seeking treatment in Turkey can achieve significant cost savings on an all-inclusive package, eliminate long waiting lists, receive high-quality assurance through international accreditations (JCI), and experience a seamless, stress-free journey from arrival to post-discharge care. This report serves as the definitive guide for those seeking a more efficient and holistic path for their health journey.
Part I: The Bariatric Surgery Landscape in Norway—Challenges and Realities
1.1 Public and Private Healthcare: A Tale of Two Systems
Access to bariatric surgery, such as gastric bypass and sleeve gastrectomy, in Norway is a complex issue with distinct differences between the public and private healthcare sectors. The public sector accommodates patients within a high-quality but heavily regulated framework, while the private sector offers a faster route but requires significant financial outlay. A health technology assessment by the Norwegian Institute of Public Health (NIPH) estimated the cost of bariatric surgery for the first year to be between 83,500 and 118,000 Norwegian Kroner (NOK) per patient. These figures, reflecting the national healthcare perspective, represent a substantial financial burden for the state. This explains why the public system manages access to surgery through restrictive criteria and bureaucratic processes.
Underpinning these restrictions is a legal framework known as the “New Method,” established in 2013, which mandates that all surgical innovations for obesity must undergo a Health Technology Assessment (HTA) before being funded. This process, which has included an evaluation of obesity surgery since 2019, was completed in March 2022. The report concluded that no definitive recommendation could be made for a preferred surgical procedure (sleeve gastrectomy, Roux-en-Y gastric bypass, etc.) for morbid obesity. It also found that the cost differences were insignificant. This bureaucratic process directly contributes to extended waiting times for patients. The cautious, evidence-based approach of the legal framework, while well-intentioned, leads to significant delays for the patient. This explains why the public system operates at such a slow pace.
1.2 The Patient Eligibility Labyrinth: When the System Says ‘No’
Access to the public healthcare system in Norway is governed by strict eligibility criteria. Traditionally, individuals must have a body mass index (BMI) of 40 kg/m² or higher, or a BMI between 35 and 40 kg/m² with high-risk comorbidities like type 2 diabetes, to be considered for bariatric surgery. These rigid thresholds exclude patients with a BMI between 35-40 who have no comorbidities or those with a BMI below 35 from surgical treatment.
This strict set of criteria stands in contrast to existing medical evidence. Research has shown that bariatric surgery can be highly effective even for patients with a BMI below 35, particularly for the remission of type 2 diabetes. While diabetic patients across a wide range of BMIs can achieve remission with surgical treatment , public policy often excludes these potential candidates. This creates a demographic known as the “in-between patient,” who is medically a good candidate but is bureaucratically locked out of the system. This group is forced to seek alternative solutions, making them a prime target for medical tourism.
1.3 The Time Cost of Care: Norway’s Waiting Lists
One of the most significant barriers for patients seeking bariatric surgery in Norway is waiting times. A report from the Scandinavian Obesity Surgery Registry (SOReg) highlights that while Sweden has a legal time limit for patients to undergo surgery within six months of referral, Norway has no such time limit regarding surgical timing. This results in the time from patient referral to surgery being longer in Norway compared to Sweden.
The uncertain waiting periods in public hospitals often drive some patients to the private sector. A private clinic can offer a surgery date within one to two weeks after the medical documents have been assessed. However, this path also has its own risks. The same SOReg report noted that the data acquisition rate for private hospitals in Norway between 2019 and 2021 ranged from only 13% to 39%. This low rate points to a lack of centralized oversight and data transparency in the private sector. This means that when a patient bypasses the uncertain waiting lists of the public system for a private clinic, they may be entering a less transparent and less accountable system. This stands in stark contrast to the situation in Turkey, which is bolstered by international accreditations and a more centralized structure.
Part II: The Turkish Solution—A New Model in Health and Wellness Travel
2.1 The Rise of Medical Tourism: Why Turkey is at the Top
In response to the complex and restrictive bariatric surgery environment in Norway, Turkey has become a leading global destination for medical tourism. Due to its strategic location and investments in the healthcare sector, Turkey is consistently ranked among the top 10 medical tourism destinations worldwide by the International Medical Travel Journal (IMTJ). The key factors behind this success include significant cost advantages compared to Western countries (with savings of up to 50-70%), internationally experienced surgeons, advanced technological infrastructure, and the absence of long waiting lists.
Turkey’s success is not accidental; it is a strategic combination of its geographical position at the crossroads of Europe and Asia , government-backed initiatives like the International Health Services Inc. (USHAŞ) , and private sector investments in modern facilities. This holistic approach has transformed Turkey from just an affordable option into a robust and multi-layered system. The 24/7 interpreting and call center for foreign patients, run by the Ministry of Health of the Republic of Turkey , is strong evidence that medical tourism is a national priority and a commitment to the field.
2.2 Beyond the Price: Defining the ‘Cure Holiday’ Experience
The term “Cure Holiday” refers to a model of medical travel that integrates a medical procedure with a supportive, often luxurious, recovery environment and opportunities for cultural exploration. This approach is designed to alleviate the stress of traditional healthcare. In this context, it is important not to confuse the term with CURE International, a Christian charity that operates a network of children’s hospitals globally. An expert report should clearly state this important distinction to avoid any misunderstanding.
A key component of the “Cure Holiday” model in Turkey is the all-inclusive package. These packages often cover essential medical services—such as VIP transfers from the airport to the hotel and hospital, hospital and hotel accommodation, pre- and post-operative tests, and surgical and anesthesia fees—as well as nutritional and follow-up support that can extend up to a year. This comprehensive model removes the burden on patients of separately organizing logistics like flights and accommodation, providing a seamless, predictable, and single-price journey rather than a stressful and fragmented process. This approach reduces the logistical and psychological burdens associated with seeking treatment abroad, making the decision more attractive and manageable.
Part III: Comparative Analysis: Norway vs. Turkey
3.1 Head-to-Head Cost Breakdown: Price vs. Value
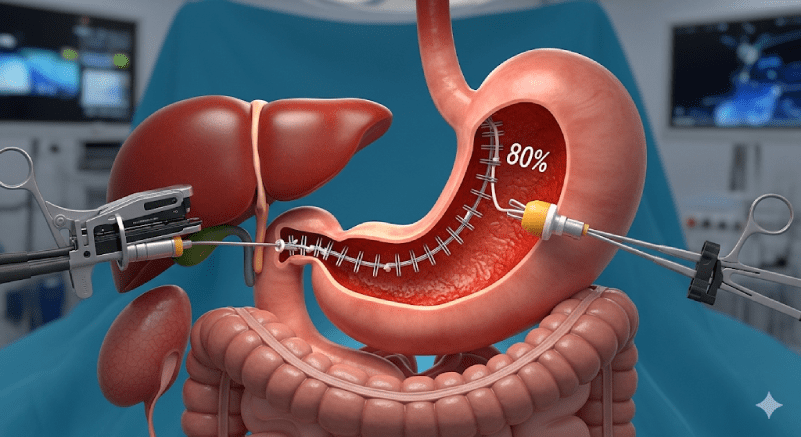
A comparison of bariatric surgery costs in Norway with the all-inclusive packages in Turkey reveals the tangible financial and experiential benefits for patients. In a private clinic in Norway, the cost of gastric sleeve surgery is approximately 100,000 Norwegian Kroner (around 8,700 Euros). This cost typically covers only the surgical procedure and limited follow-up. While the public system eliminates the financial cost for the patient, it imposes unseen costs such as comorbidities and waiting times.
In contrast, the cost of all-inclusive gastric sleeve packages in Turkey ranges from 3,500 to 12,000 USD (approximately 3,250 to 11,000 Euros).
Table 1: Comparative Gastric Sleeve Costs and Coverage (Norway vs. Turkey)
| Features | Norway (Private) | Norway (Public) | Turkey (All-Inclusive) |
| Cost | ≈ 100,000 NOK | Covered by the state; no cost to the patient | 3,500 – 12,000 USD |
| Included Services | Surgery, limited follow-up | Surgery, follow-up | Surgery, hospital fees, transfers, hotel accommodation, all tests, medications, 1-year follow-up |
| Waiting Time | Variable (can be fast, but data transparency is low) | Uncertain; no legal time limit | None; fast scheduling and appointments |
| Follow-up and Post-op Support | Limited; generally includes standard procedures | Includes long-term follow-up | Often includes remote nutritional and follow-up support for up to 1 year |
This table illustrates not just the price difference but also the value offered by each option. The Norwegian option presents a medical procedure with a financial transaction, while the Turkish option provides a comprehensive experience that bundles logistical and recovery services into a single, transparent package for the patient. This embodies the “Cure Holiday” concept and makes its value proposition undeniable.
3.2 Efficiency of Access: Waiting Times
In terms of access efficiency, the difference between Norway and Turkey is stark. In Norway, there is no legal time limit for bariatric surgery waiting times. This subjects patients in the public system to an uncertain waiting period, increasing the risk of worsening obesity-related comorbidities.
Clinics in Turkey directly address this key issue. The medical tourism infrastructure is optimized for rapid access to medical procedures, including gastric sleeve surgery. Patients can schedule their surgery quickly, without encountering waiting lists. This stands in sharp contrast to the Norwegian public system, which puts patients in a state of indefinite waiting, while the Turkish model democratizes access to speed and makes it a standard part of the patient journey.
3.3 Patient Experience: A Holistic Perspective
Turkey sets itself apart by focusing on every aspect of the patient experience. The all-inclusive packages ensure that everything from airport arrival to post-discharge recovery is seamlessly coordinated. Many clinics have English-speaking medical and support staff. This is further reinforced by the Republic of Turkey Ministry of Health’s 24/7 interpreting and call center for foreign patients , a service that provides an extra layer of reassurance from the state. This service demonstrates that medical tourism is not just a private endeavor but a national priority, significantly contributing to patient confidence.
Part IV: Addressing Concerns—Quality, Safety, and Post-operative Care
4.1 Upholding International Standards and Accreditations
The lower cost of surgery in Turkey might lead some patients to worry about a compromise on quality. However, the reality is quite the opposite. Turkish healthcare facilities have invested heavily in aligning with international standards. Turkey is the second country globally with the most Joint Commission International (JCI) accreditations. JCI accreditation is considered the “gold standard” in global healthcare, requiring a rigorous evaluation of over 1,300 criteria, including patient safety, hygiene, and staff qualifications. Hospitals in Turkey are also audited by the Ministry of Health and may hold ISO certifications. This multi-layered system of oversight and assurance directly refutes the common misconception that a lower price equals lower quality.
4.2 Post-operative Care Process and Follow-up Services
The all-inclusive model in Turkey provides a comprehensive care process that continues long after the patient is discharged. The patient journey begins with an airport greeting, followed by hospital admission for extensive pre-operative tests, including blood work, endoscopy, and ECG. After surgery, patients typically stay in the hospital for 1-3 nights before being discharged to a high-quality hotel for a few more days of rest.
Upon discharge, the patient is given detailed instructions on a progressive diet plan, starting with liquids and slowly transitioning to solid foods. Adherence to this post-operative diet is critical for preventing complications and promoting healing. This structured journey ensures the patient is not left to navigate the recovery process alone and is a vital factor for successful and sustainable weight loss.
4.3 Long-Term Support: Continuity for International Patients
Bariatric surgery is not a one-time event but the beginning of a journey that requires permanent lifestyle changes. Clinics in Turkey understand the importance of long-term follow-up for international patients. Packages offer months of online follow-up and nutritional counseling even after the patients return home. Most packages include up to a year of follow-up and dietitian support. This is a critical component of the bariatric surgery model in Turkey. It demonstrates that the clinic is invested in the patient’s long-term health, cementing the procedure’s connection to successful and sustainable weight loss. This approach directly addresses one of the biggest concerns for patients considering surgery abroad.
Conclusion: A Healthier Future Awaits You
The analysis in this report demonstrates that while Norway offers a high-quality public and private system for bariatric surgery, it is a system riddled with significant barriers such as high costs, strict eligibility criteria, and long waiting times. These obstacles prevent many patients from accessing the timely care they need and deserve.
In contrast, Turkey presents a superior, more accessible, and more comprehensive solution to these challenges. The “Cure Holiday” model redefines the patient experience by bundling cost-effectiveness, rapid access, transparent packages, and a globally accredited, patient-centered approach. The lower cost in Turkey does not imply a compromise on quality; rather, it is a result of a robust system of accreditations and support, reflecting the country’s strategic commitment to health tourism. The risk and uncertainty a patient in Norway faces in a complex and fragmented healthcare system are eliminated by Turkey’s all-inclusive model, which offers a seamless, stress-free, and secure journey.
In summary, for Norwegian patients considering gastric sleeve surgery, Turkey is more than just a more affordable alternative; it is a safer, more efficient, and more holistic path to taking control of one’s health. The first step towards a healthier life is no longer a distant, bureaucratic aspiration but an accessible reality.