What is Radiotherapy?
Radiotherapy is a powerful method used in cancer treatment and is commonly known as “radiation therapy” in the public. This treatment involves using high-energy radiation beams to kill or stop the growth of cancer cells. Radiation damages DNA, causing cancer cells to lose their ability to divide and multiply. Although the healthy cells in our body are also affected by this radiation, they can repair the damage more easily than cancer cells. For this reason, the treatment process is usually planned at specific intervals to allow healthy cells to recover. Radiotherapy can be used as a primary treatment alone, or it can be applied before a surgical operation to shrink a tumor or after surgery to destroy any remaining cancer cells. Additionally, it can be used in combination with other cancer treatments like chemotherapy to increase the effectiveness of the treatment.
The History and Development of Radiotherapy
The history of radiotherapy begins in the late 19th century with the discovery of X-rays and radioactivity. Wilhelm Conrad Röntgen’s discovery of X-rays in 1895, followed by Henri Becquerel, Pierre, and Marie Curie’s discovery of radioactivity, constituted the first steps in this field. In the early 20th century, the destructive effect of radiation on cancer cells was noticed, and radiotherapy began to be applied with primitive devices. However, because the devices of that era were not very precise and side effects were high, the treatment remained limited. The real development occurred in the 1950s with the emergence of linear accelerators (LINAC). These devices added more precision and safety to the treatment by producing higher energy levels of radiation. Today, thanks to advances in computer technology, radiotherapy devices can be precisely aimed to deliver the maximum dose to the tumor while minimizing damage to healthy tissues.
The Working Principle of Radiotherapy: How Cancer Cells Are Destroyed
The basic working principle of radiotherapy is to damage the DNA of cancer cells. High-energy radiation beams cause breaks in the DNA double helix of cells. While normal cells have mechanisms to repair this damage, cancer cells lack this repair ability due to their flawed genetic structure. This accumulation of damage causes cancer cells to lose their ability to divide and multiply, ultimately leading to their death. Although radiotherapy targets cancer cells, the surrounding healthy tissues are also partially affected by this process. However, because healthy tissues regenerate and repair damage faster, side effects are usually temporary. The treatment is generally spread over a period of weeks, allowing healthy cells to regenerate.
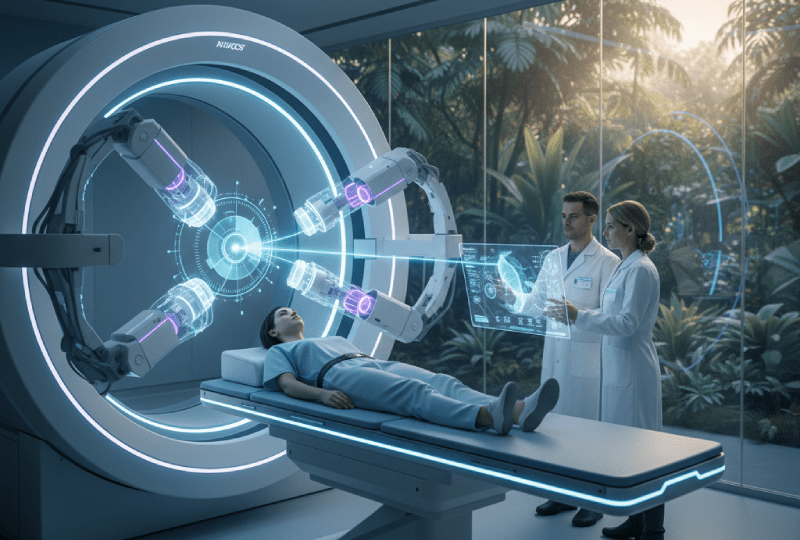
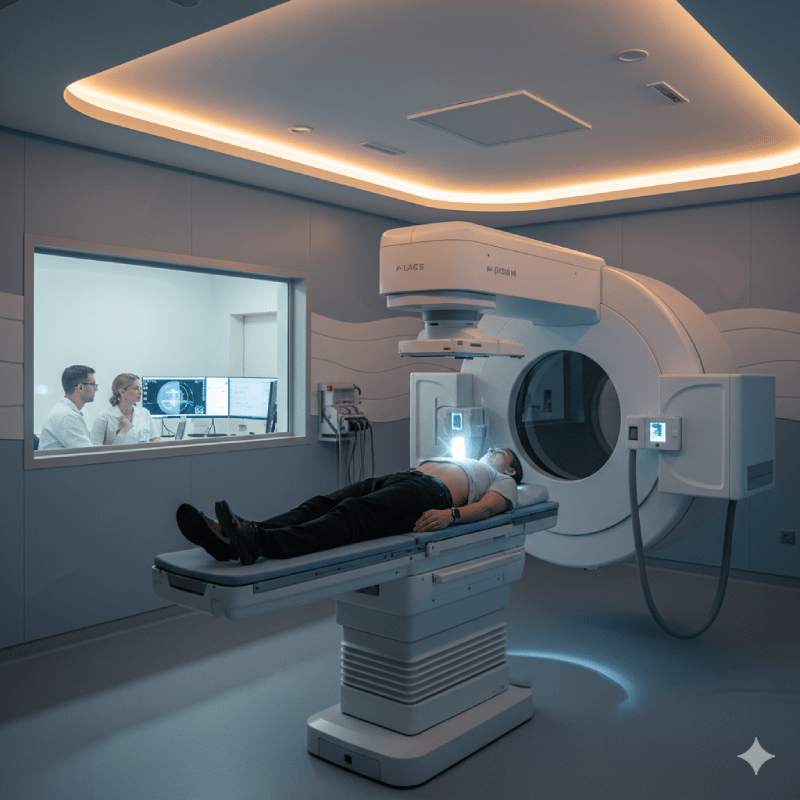
External Radiotherapy (External Irradiation)
External radiotherapy is the most commonly used type of radiotherapy. In this method, the area where the tumor is located is targeted with high-energy beams from outside the body by a large machine called a linear accelerator (LINAC). The patient lies on a special table during treatment, and the machine rotates around the tumor to irradiate it from different angles. In this way, the tumor is exposed to a high dose as it is at the intersection point of the beams coming from different angles, while healthy tissues receive lower doses and are protected. This treatment method can be used for tumors in almost any part of the body and is the most common form of radiotherapy.
Brachytherapy (Internal Irradiation)
Brachytherapy is a type of radiotherapy where the radiation source is placed directly inside or near the tumor. This allows a very high dose of radiation to be delivered to the cancer cells, while minimizing damage to the surrounding healthy tissues. Brachytherapy is highly effective in the treatment of certain types of cancer such as prostate, uterine, and breast cancer. The treatment can be applied permanently or temporarily. In permanent brachytherapy, small radioactive seeds are placed inside the tumor and slowly emit radiation to destroy the tumor. In temporary brachytherapy, the radiation source is placed for a short period and removed after treatment.
Systemic Radionuclide Therapy
Systemic radionuclide therapy is a method where a radioactive substance is injected intravenously or taken orally and distributed throughout the entire body. This radioactive substance targets and destroys cancer cells from within. The most well-known example is radioactive iodine (I-131) therapy used in the treatment of thyroid cancer. Since iodine is absorbed by thyroid cells, radioactive iodine reaches and destroys the cancerous thyroid cells. This method can also be effective in treating cancer cells that have spread to different parts of the body (metastasized).
The Radiotherapy Planning Process: The First Steps
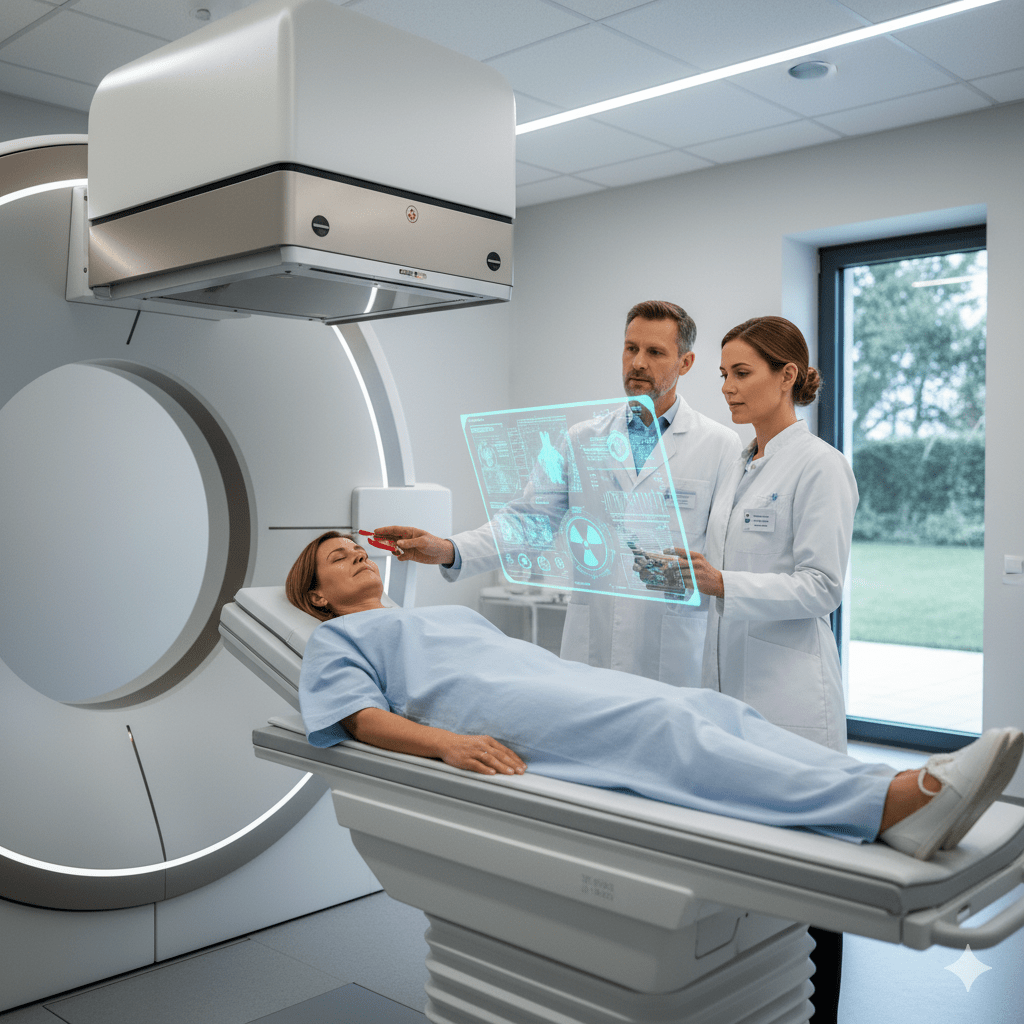
Before starting radiotherapy treatment, the patient must undergo a detailed planning process. This process is of critical importance for the success of the treatment and for minimizing side effects. First, the patient is evaluated by a team consisting of a radiation oncologist, a medical physicist, and a radiotherapy technician. This team determines the most suitable treatment strategy by considering the patient’s general health condition, the location, size, and type of the tumor. This evaluation ensures that the treatment is personalized.
CT (Computed Tomography) Simulation
One of the most important steps in the planning process is CT simulation. This is a process where a three-dimensional map of the tumor and the surrounding healthy organs is created with the patient in the treatment position. During the CT simulation, the patient is positioned exactly as they will be during the treatment sessions. Small tattoos or marks are placed on the body to ensure the same position is maintained before each session. These images are used by the radiation oncologist and medical physicist to determine the exact location of the tumor and to plan how to protect healthy tissues.
Treatment Plan and Dosimetry
After the CT simulation, the medical physicist creates a treatment plan based on the tumor’s map. At this stage, the exact amount of radiation dose to be given to which areas is precisely calculated. This is called dosimetry. Dosimetry aims to target the maximum dose to the entire tumor while minimizing the dose to the heart, lungs, spinal cord, or other critical organs. This plan determines the angles, duration, and intensity of the radiation for each session.
Volumetric Modulated Arc Therapy (VMAT)
VMAT is one of the most advanced methods in modern radiotherapy technology. In this technique, the linear accelerator (LINAC) machine rotates in a continuous arc around the patient to perform irradiation. As the machine rotates, it continuously changes the intensity of the radiation. This allows for a precise adjustment of the radiation dose according to the three-dimensional shape of the tumor. The biggest advantage of VMAT is that it significantly shortens the treatment time and increases healthy tissue protection. The short treatment time makes it easier for the patient to remain still on the treatment table.
Radiotherapy Devices: Linear Accelerator (LINAC)
The Linear Accelerator (LINAC) is the main device used in external radiotherapy. This machine accelerates electrons to produce high-energy X-rays or electron beams. These beams are directed to the tumor area through a computer-controlled system. Modern LINACs have advanced technologies that can work with millimeter precision, controlling the intensity and shape of the beams. This allows for irradiation based on the shape of the tumor, and healthy tissue damage is minimized.
Targeted Therapy: IMRT and IGRT
Intensity-Modulated Radiotherapy (IMRT) is a technique that adjusts the intensity and shape of the radiation according to the three-dimensional shape of the tumor. In this way, different doses of radiation can be given to different parts of the tumor. This provides a great advantage, especially in the treatment of tumors that are irregular in shape or are close to critical organs. Image-Guided Radiotherapy (IGRT) is a technology that verifies the position of the tumor before each session. After the patient is positioned on the table, the machine takes a new image of the tumor and compares it with the initial planning image. Thus, even small changes in the tumor’s position can be detected, increasing the precision of the treatment.
Stereotactic Body Radiotherapy (SBRT)
Stereotactic Body Radiotherapy (SBRT) is a method used in the treatment of small and isolated tumors, where a high dose of radiation is delivered in a short period. SBRT can be used in patients who are not suitable for surgery or as an alternative to surgery. This treatment is usually completed in a short period, such as 1-5 sessions. Because it focuses on the target with high precision, the healthy tissues around the tumor are protected to the maximum extent. It is frequently preferred in the treatment of tumors in areas such as the lungs, liver, and spine.
Proton Therapy: The Technology of the Future
Proton therapy is one of the most advanced technologies in radiotherapy. In this method, protons are used instead of photon beams. The biggest advantage of protons is that their energy can be released at a specific depth, which is exactly within the tumor. Protons cause little damage to the healthy tissue in front of the tumor and no damage to the tissue behind the tumor. This feature makes a big difference, especially in the treatment of tumors in children or in sensitive areas such as the spinal cord. Unfortunately, there are no proton therapy centers in Turkey at the moment, and it may be necessary to go abroad for this treatment.
How are Radiotherapy Sessions Conducted?
Radiotherapy sessions are generally painless and quick. Before each session, the patient is laid on the treatment table and brought to the position determined in the treatment plan. Laser lights and small marks made on the body are used to correctly adjust this position. When the session begins, the machine starts working and delivers radiation to the tumor area. The patient remains alone in a room during this time, but the technicians and doctors are in constant contact with the patient via a camera and audio communication. Nothing is felt during the irradiation. The sessions usually last 15-20 minutes.
Treatment Duration and Number of Sessions
The duration of radiotherapy treatment varies depending on the type and stage of cancer, the size of the tumor, and the patient’s general health condition. Generally, the treatment is applied in sessions five days a week, lasting for several weeks. The total number of sessions can vary between 20 and 40. This distribution allows normal tissues to repair damage and increases the cumulative effect of the radiation. Sometimes, especially in palliative (symptom-relieving) treatments, the number of sessions may be fewer.
Patient Comfort and Safety in Radiotherapy
During radiotherapy, the patient’s comfort and safety are kept at the highest level. The treatment table is specially designed to help the patient maintain the correct position. Breath control and other special techniques may be used to limit tumor movement. Throughout the treatment, the patient is continuously monitored by technicians. In case of any discomfort or concern, the patient can communicate with the team via the audio communication system, and the treatment can be stopped. Modern machines ensure that the radiation dose is precisely adjusted, preventing unnecessary radiation exposure.
Potential Side Effects of Radiotherapy
The side effects of radiotherapy vary depending on the area being irradiated and the radiation dose. The most common side effects include fatigue, skin redness, itching, or peeling. Radiotherapy applied to the abdominal area can lead to digestive problems such as nausea, vomiting, or diarrhea. Treatments to the head or neck area may cause dry mouth, difficulty swallowing, or changes in the sense of taste. These side effects are usually temporary and gradually disappear after the treatment is completed. Doctors and nurses provide recommendations to the patient to manage these side effects and initiate medication if necessary.
Radiotherapy and Chemotherapy: Combined Treatment
The use of radiotherapy and chemotherapy together is called chemoradiation. These two treatment methods can increase the success of cancer treatment by enhancing each other’s effects. Chemotherapy can make tumor cells more sensitive to radiation, which makes radiotherapy more effective. This combined treatment is a standard approach for certain types of cancer, especially head and neck cancers, lung cancer, and rectal cancer. Although chemoradiation increases side effects compared to treatments applied alone, the results are generally more successful.
Palliative Radiotherapy: Improving Quality of Life
Palliative radiotherapy is a type of treatment applied to relieve cancer symptoms and improve the patient’s quality of life. This treatment is used in cases where the cancer is advanced and its complete elimination is not possible. For example, palliative radiotherapy can be applied to relieve pain in tumors that have spread to the bones and cause severe pain, to control neurological symptoms caused by brain metastases, or to shrink a tumor that is blocking the airways to facilitate breathing. These treatments are usually shorter and completed in a few sessions.
Follow-up and Control After Radiotherapy
After radiotherapy treatment is completed, the patient is taken into a regular follow-up and control process. These follow-ups are vital for evaluating the effectiveness of the treatment and managing possible late side effects. Controls usually involve a physical examination and imaging methods such as blood tests, MRI, CT, or PET/CT. These follow-ups help to monitor whether the cancer has recurred or if new side effects have developed.
Integration of Radiotherapy with Other Treatments
Radiotherapy can be used in combination with many different cancer treatment methods, such as surgery, chemotherapy, immunotherapy, and targeted therapies. The order and combination of these treatments are determined based on the type and stage of cancer. For example, in some cases, radiotherapy is done to shrink a tumor before surgery, while in others, it can be applied after surgery to destroy any remaining cancer cells. This integrated approach ensures that cancer treatment is planned in a versatile and personalized manner.
Radiotherapy Centers and Quality Standards in Turkey
Turkey has highly developed centers in the field of radiotherapy. Modern linear accelerator devices and advanced planning technologies (IMRT, VMAT, IGRT) are available in large cities and university hospitals. The Ministry of Health requires these centers to meet certain quality standards. Before starting treatment, it is important to ensure that the center you choose has modern equipment and works with an experienced team. You can do research on this subject and look at the references and patient reviews of the centers.
Treatment Options and Choosing a Specialist Doctor
Choosing a radiation oncologist for radiotherapy treatment is a critical step for the success of the treatment process. It is important that the doctor you choose is experienced in your type of cancer and informs you in detail about the treatment options. Discuss all your questions openly with your doctor: Get answers to questions like why the treatment is necessary, which device will be used, what the potential side effects are, and how long the treatment will last. Also, getting a second opinion from a specialist can always be beneficial.
Social Security and Insurance Coverage
In Turkey, radiotherapy treatments are generally covered by the Social Security Institution (SGK). You can benefit from these treatments in hospitals affiliated with SGK and in private hospitals that have an agreement with SGK. Private insurance policies may also cover the costs of radiotherapy, depending on the scope of the policy. Before starting treatment, it is important to find out if the hospital has an agreement with SGK or your private insurance and how much of the treatment costs will be covered. This will help minimize financial concerns during the treatment process.